Factors affecting marginal integrity of class II bulk-fill
composite resin restorations
J Dent Res Dent Clin Dent Prospects, 11(2), 101-109; DOI:10.15171/joddd.2017.019
Clinical Dentistry
Factors affecting marginal integrity of class II bulk-fill
composite resin restorations
Siavash Savadi Oskoee1, Mahmoud Bahari1,2*, Elmira Jafari Navimipour1, Amir Ahmad Ajami1, Negar Ghiasvand3, Ayda Savadi Oskoee1
1
Department of Operative Dentistry, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
2
Dental and Periodontal Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3
Department of Operative Dentistry, Faculty of Dentistry, Urmia University of Medical Sciences, Urmia, Iran
*Corresponding Author; Email: mahmoudbahari@ymail.com
© 2017 by Tabriz University of Medical Sciences
Abstract
Background. Bulk-fill composite resins are a new type of resin-based composite resins, claimed to have the capacity to be
placed in thick layers, up to 4 mm. This study was carried out to evaluate factors affecting gap formation in Cl II cavities
restored using the bulk-fill technique.
Methods. A total of 60 third molars were used in this study. Two Cl II cavities were prepared in each tooth, one on the
mesial aspect 1 mm coronal to the CEJ and one on the distal aspect 1 mm apical to the CEJ. The teeth were divided into 4
groups: A: The cavities were restored using the bulk-fill technique with Filtek P90 composite resin and its adhesive system
and light-cured with quartz tungsten halogen (QTH) light-curing unit. B: The cavities were restored similar to that in group
A but light-cured with an LED light-curing unit. C: The cavities were restored using the bulk-fill technique with X-tra Fil
composite resin and Clearfil SE Bond adhesive system and light-cured with a QTH curing unit. D: The cavities were restored
similar to that in group C but light-cured with an LED light-curing unit. The gaps were examined under a stereomicroscope
at ×60. Data were analyzed with General Linear Model test. In cases of statistical significance (P<0.05), post hoc
Bonferroni test was used for further analyses.
Results.
The light-curing unit type had no effect on gap formation. However, the results were significant in relation to the
composite resin type and margin location (P<0.001). The cumulative effects of light-curing unit*gingival margin and lightcuring
unit*composite resin type were not significant; however, the cumulative effect of composite rein type*gingival margin
was significant (P=0.04)
Conclusion.
X-tra Fil composite exhibited smaller gaps compared with Filtek P90 composite with both light-curing units.
Both composite resins exhibited smaller gaps at enamel margins.
Keywords: Composite resin, bulk fill, curing light, marginal gap, silorane, methacrylate.
© 2017 Savadi Oskoee et al. This is an Open Access article published and distributed by Tabriz University of Medical Sciences under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Despite great advances in the field of composite resin technology and extension of its applications in restorative dentistry, they still have disadvantages, including high wear rate, low strength, technique sensitivity and more importantly, polymerization shrinkage that gives rise to gap formation at the restorative material‒cavity wall interface, leading to microleakage due to the internal and interfacial stresses it creates.1 Microleakage leads to recurrent caries, postoperative sensitivity, marginal discoloration and loss of the restoration.2,3 Therefore, a large number of studies have been undertaken on techniques that result in a decrease in polymerization shrinkage, including placement of composite resins using the incremental technique, use of materials with low elastic modulus to absorb stresses and use of techniques to decrease the C-factor.4-7 Since these techniques are time-consuming and increase the chair time, resin-based composite (RBC) manufacturers have made significant developments to reduce the shrinkage stress generated on light irradiation and today dentistry boasts of RBC filler technology that encompasses nanotechnology,8 polymerization modulators technology9 and non-methacrylate-based monomeric resin formulations.10
One of these non-methacrylate-based monomeric resin formulations is silorane-based composite resins which are a combination of siloxane and oxirane under a cationic ring-opening polymerization.11,12 The silorane-based composite resins undergo volumetric shrinkage of 0.99%,13 which is significantly less than that of methacrylate-based composite resins (2.9‒7.1%).14 Compared to methacrylate-based composite resins, in silorane-based composite resins, polymerization stresses are compensated by opening an oxirane ring element.15 Opening of oxirane rings during polymerization compensates the volumetric decrease resulting from packing of the monomers.16 In relation to silorane-based composite resins, evaluation of the cohesive bond of the incremental layers has shown that the layers of this type of composite resin exhibit poorer cohesive bond properties compared to dimethacrylate composite resins due to the absence of oxygen-inhibited layer and a different polymerization mechanism. It is advisable to use the bulk-fill technique to place such composite resins in the cavity.17
Other products are bulk-fill methacrylate-based composite resins using polymerization modulator technology specially designed for bulk-filling technique. By changing the initiator in these composite resins it has become possible to place composite resin at thicknesses greater than 4 mm, which results in significantly shorter chair times during the restorative procedures.9 It has also been shown that the depth of cure at these thicknesses is greater than that in nanofilled composite resins with the same thickness.18
Palin et al19 demonstrated that the microleakage of a Class V cavity restored with a silorane-based composite resin was not significantly different from that of a similar cavity restored with a conventional methacrylate-based composite. On the other hand, a number of studies have shown that silorane-based composite resins exhibit significantly lower shrinkage forces, less microleakage and better marginal adaptation than conventional methacrylate-based composite resins.20,21
EL-Damanhoury and Platt showed that bulk-filled composite resins have significantly less polymerization shrinkage compared to conventional posterior composite resins.4 However, according to Heintze et al,22 no significant differences were detected between the marginal quality of composite resin restorations placed in bulk and those placed in three increments.
At present, the chief concern about curing bulk-fill composite resins is the amount of polymerization shrinkage and the subsequent gap formation. Such shrinkage is more important at cervical margins of proximal boxes.23 Moorthy et al24 showed that the bulk-fill flowable RBC bases resulted in a significant decrease in cuspal deflection compared to a conventional RBC restored in an oblique incremental filling technique with no change in cervical microleakage.
The present study was undertaken to evaluate the effect of the type of light-curing unit and the location of the gingival margin, i.e. enamel and dentinal margins, on gap formation in Cl II cavities restored with bulk-fill silorane- and methacrylate-based composite resins. The null hypothesis of the study stated that the type of composite resin, light-curing unit and gingival margin location has no effect on gap formation.
Methods
Sixty third molars without caries and defects were selected after surgical extraction due to impaction or semi-impaction. The teeth were cleansed with scaling curettes and immersed in 0.5% chloramine solution (Kemika, Zagreb, Croatia) for one month. Then two standard Cl II MO and DO cavities were prepared in the teeth using a #4 round diamond and a #245 fissure bur (Mani Inc, Utsuno-miya, Tochigi, Japan) in a high-speed handpiece (NSK, Tochigi-Ken, Japan) under air and water spray. One new bur was used for each eight cavities. The cavities measured 2.0 mm in the occlusal isthmus depth, 5.0 mm in the buccolingual width of the proximal box in the occlusal area, 5.5 mm in the gingival area, 2.5 mm in the depth of the axial wall in the occlusal area and 1.5 mm in the gingival area; in addition, the box height was 1 mm occlusal to the CEJ on the mesial aspect and 1 mm apical to the CEJ in the distal aspect. The dimensions mentioned above were confirmed with the use of a #15 UNC periodontal probe. Bevels were not placed at the cavosurface margins.
The teeth were randomly assigned to 4 groups with 15 teeth or 30 cavities in each group. The mesial and distal cavities of all the samples were etched for 15 seconds, rinsed and dried with cotton pellets.
Group A: Filtek P90 composite resin (FS) and quartz-tungsten-halogen (QTH) light-curing unit
First the P90 system self-etch adhesive primer (3M ESPE, St. Paul, MN, USA) was applied to the cavity walls with a microbrush, following manufacturer’s instructions, followed by the application and curing of P90 system adhesive bond for 10 seconds (3M ESPE, St. Paul, MN, USA). Then the cavities were restored with Filtek P90 composite resin (3M ESPE, St. Paul, MN, USA) using the bulk-fill technique and light-cured with the QTH light-curing unit.
Group B: Filtek P90 composite resin and light emitting diode (LED) light-curing unit
The cavities were restored in a manner similar to that in group A except that an LED light-curing unit was used in this group.
Group C: X-tra Fil composite resin and QTH light-curing unit
First the Clearfil SE Bond (Kuraray, Osaka, Japan) self-etch system was applied to the cavity walls with a microbrush, following manufacturer’s instructions, and cured for 10 seconds. Then the cavities were restored with X-tra Fil composite resin (VOCO Gmbh, Cuxhaven, Germany) using the bulk-fill technique and light-cured with the QTH light curing unit.
Group D: X-tra Fil composite resin and LED light-curing unit
The cavities were restored in a manner similar to that in group C except that an LED light-cuing unit was used in this group.
QTH Astralis 7 (Ivoclar, Vivadent, Lichtenstein) and LED Demetron A2 (Kerr, Donbury, Italy) were used for light-curing of composite resins at a light intensity of 1000 mW/cm2 for 20 and 10 seconds, respectively. Table 1 presents the particulars of the materials used in the present study.
|
Table 1. Material used and their composition
|
| Material |
Type |
Composition |
Batch No |
Manufacturer |
Application mode |
| Filtek P90 (silorane) |
Matrix expanding Composite |
Silane treated quartz ;yttrium trifluride; Bis-3,4-Epoxycyclohexyl-phenyl-Methysilane ;3,4-Epoxycyclohexylcyclo-Polymethylsiloxane |
N384451 |
3M ESPE, St Paul, MN, USA |
Bulk fill technique |
| X-tra Fil |
Bulk-fill restorative |
MMA, Bis EMA, Inorganic fillers |
1147096 |
Voco, Cuxhaven, Germany |
Bulk fill technique |
| Silorane adhesive |
|
Primer: phosphorylated methacrylates, vitrebond copolymer, bis-GMA, HEMA, water, ethanol, silane-treated silica filler, initiators, stabilizers
Bond: hydrophobic dimethacrylate, phosphorylated methacrylates, TEGDMA, silane treated silica filler, initiators, stabilizers |
N213019
N213052 |
3M ESPE, St Paul, MN, USA |
Apply primer to tooth surface ;gently air dry the surface and light cure for 10 s; apply bond ;gently air dry and light cure for 10s |
| Clearfil SE Bond |
|
Primer: MDP, HEMA, hydrophilic dimethacrylate, photoinitiator, water
Bond:10-MDP,bis GMA,HEMA hydrophilic dimethacrylate, microfiller, photoinitiator |
1039AA
1550AA |
Kurary Medical Inc, Okayama, Japan |
Apply primer to tooth surface; air dry for 10s;applay bond; dry for 10 s and light cure for 10s. |
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
Abbreviations: MMA: Methyl methacrylate, Bis EMA: Bisphenol A polyetheylene glycol diether dimethacrylate, Bis GMA: Bisphenol-A-glycidyl methacrylate, UDMA: Urethane dimethacrylate, TEGDMA: Triethyleneglycol dimethacrylate, HEMA:2-hydroxyethyl methacrylate, MDP: Methacryloxydecyl dihydrogen phosphate
|
|
The results showed that the composite resin type affected gap formation, and the size of gaps with the X-tra Fil composite resin was smaller than that with the silorane-based composite resin at both enamel and dentin margins, irrespective of the type of the light-curing unit.
|
All the restorations were finished with finishing disks containing aluminum oxide from coarse to fine (Sof-Lex TM, 3M ESPE, St. Paul, USA) based on manufacturer’s instructions. The samples were incubated (Irankhodsaz Co., Tehran, Iran) in distilled water at 37°C for 1 week, followed by thermocycling under standard conditions (5/55±5°C, 500 cycles).
Subsequently, the teeth were bisected mesiodistally using diamond disks (Diamond GmbH, D&Z, Berlin, Germany) and marginal adaptation was evaluated under a stereomicroscope (SMZ 800, Nikon, Tokyo, Japan) at ×60. Selected areas underwent a digital radiographic procedure with the use of a digital imaging system (DS Camera Control Unit, DS-LZ Ver. 4.4) and transferred to a computer to measure gaps. A software program (DS Camera Control Unit, DS-LZ Ver. 4.4) was used to measure the width of the interfacial gaps at 3 points and their mean was recorded in µm as the mean gap size (Figure 1). Data were analyzed with SPSS 20, using the General Linear Model (GLM) multivariate variance analysis. Bonferroni post hoc tests were used for pair-wise comparisons. Statistical significance was set at P<0.05.
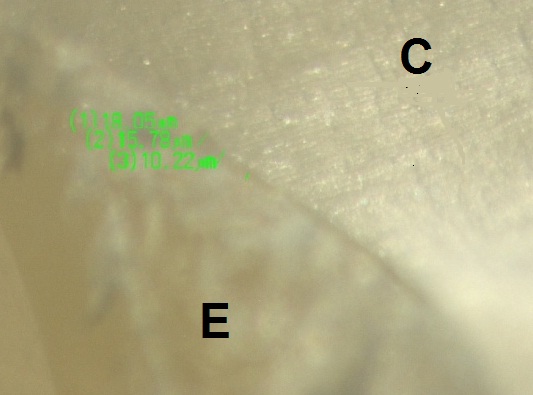
Figure 1. Sample micrograph of gap measurements (E: enamel, C: composite).
Results
Table 2 presents the mean gap sizes (µm) in the study groups.
|
Table 2. Mean gap measurements in the study groups (µm)
|
|
Composite resin type
|
Margin location
|
Light-curing unit
|
|
LED
|
QTH
|
|
X-tra Fil
|
Enamel |
7.07A |
7.21A |
|
Dentin |
11.46b |
12.07b |
|
Filtek P90
|
Enamel |
7.74C |
7.96C |
|
Dentin |
13.02d |
13.28d |
|
The differences between dissimilar letters are significant (P<0.05).
|
The results of GLM analysis showed significant differences between the two composite resin types (P<0.001) and between the two margin types (P<0.001); however, the differences between the two light-curing units were not significant (P=0.97). Evaluation of the interactive effects of variables with the use of GLM analysis showed no significant interactive effect of composite resin type‒light-curing unit (P=0.14) (Figure 2), margin location‒light-curing unit (P=0.27) (Figure 3) and composite resin‒light-curing unit‒margin type (P=0.22). However, the interactive effect of composite resin‒margin was statistically significant (P=0.04) (Figure 4).
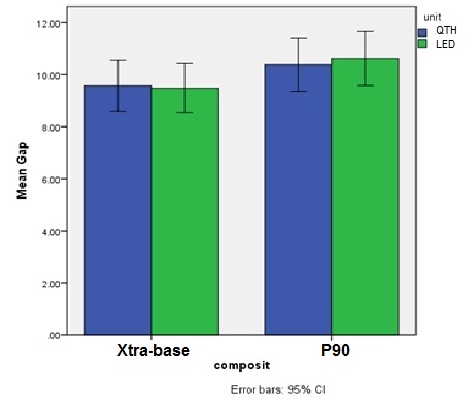
Figure 2.The error bars of the cumulative effect of composite resin‒light curing unit.
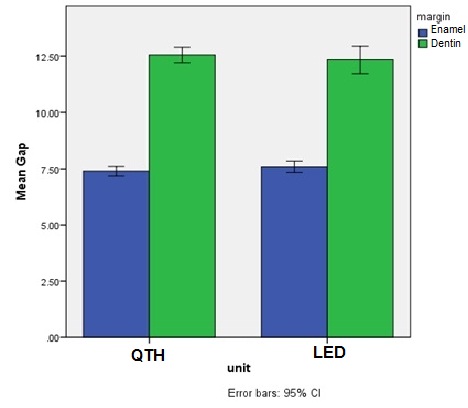
Figure 3.The error bars of the cumulative effect of margin location‒light curing unit.
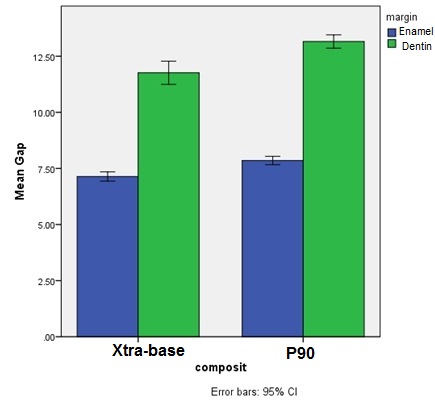
Figure 4.The error bars of the cumulative effect of composite resin‒margin location.
Two-by-two comparisons using Bonferroni post hoc test showed that the gaps with the use of silorane-based composite resin were larger than those with the use of X-tra Fil composite resin (P<0.001), with larger gaps at dentinal margins compared to the enamel margins (P<0.001). X-tra Fil composite resin exhibited smaller gaps at both enamel and dental margins with both LED and QTH light-curing units compared to the silorane-based composite resin (P<0.001).
Discussion
Contrary to incremental insertion technique in which composite resins are placed in 2-mm-thick layers in the cavity to decrease polymerization shrinkage and achieve proper depth of cure,25,26 in the bulk-fill technique composite resin is placed in 4‒6-mm layers in the cavity, saving considerable time during restorative procedures due to the restoration of the cavity in one step.
The longevity of a composite resin restoration depends on several factors, including the composite‒cavity interfacial seal.27 In cases in which there is inadequate bonding to tooth structures, forces resulting from polymerization shrinkage might give rise to gap formation at cavity wall‒restorative material interface.28 Composite resin marginal integrity might be affected by various factors, including the cavity size, the angle at which enamel prisms and dentinal tubules are cut based on their location, the procedure in which dental hard tissues are conditioned, the layering protocol and the polymerization technique used, etc.29 Therefore in the present study, the effects of composite resin type, light-curing unit type and the gingival margin location on gap formation were evaluated in Cl II restorations with the use of the bulk-fill restorative technique.
Similarly, Van Ende et al30 demonstrated that the type of the bulk filling composite has a great effect on bonding efficacy. They postulated that differences in bond strength between composites can be attributed to differences in shrinkage stress. Shrinkage stress is not a material’s property, but is inherent to the compliance and C-factor. However, in the present study standard class II cavities with similar dimensions were prepared; therefore, the C-factor was similar in all the samples. Therefore, it appears that differences in the polymerization mechanisms are responsible for differences in gap formation between these two different types of composite resin. Bulk-fill composite resins, such as X-tra Fil, have been designed for placement in 4-mm or thicker increments and it has been shown that the amount of polymerization shrinkage is low and acceptable at this thickness.
Bulk-fill composite resins exhibit a greater depth of cure and lower polymerization shrinkage compared to conventional composite resins, which is attributed to the chemical embedding of ‘polymerization modulators’ in the polymerizable resin backbone of the resin monomer, delaying the gel point. In the pre-gel phase, the polymer chains are very flexible, allowing the material to flow from the free surface of the cavity. The developing polymer’s viscosity is still low; therefore, shrinkage stress is compensated by the plastic flow during the pre-gelation phase. As a result, the internal stresses within the material are relaxed.31 The time at which the material can no longer compensate the polymerization contraction (the time until gelation) determines the final tensions in the material. However, compared to conventional methacrylate-based materials, this type of composite resins behaves differently, with a delayed gelation point, statistically similar to silorane-based composite resins only.32
The slow polymerization of the resin is another mechanism that compensates stresses in composite resins; it increases the resin’s flow capacity.33 Based on previous reports, silorane composite resins have a slower initiation of polymerization reaction and more time is necessary for formation of cations.19,34 Compared to conventional methacrylate-based composite resins, the shrinkage stress in silorane composite resins is significantly lower and the gelation time is significantly longer.
Furthermore, Van Ende et al35 reported that bulk-filling with Filtek Silorane significantly decreases the bond strength, suggesting that factors other than polymerization shrinkage may influence its bond strength. Only when FS was used in three layers and cured separately, an equally high µTBS was measured compared to conventional and low-shrinkage methacrylate-based composite resins. When FS was applied in bulk, a significantly lower bond strength was recorded. The higher bond strength of FS upon layering might be attributed to more effective polymerization of thinner layers. Additionally, several studies have reported lower hardness at the bottom of the cavity with the use of silorane composite resins in bulk.36,37 In this regard, based on a recent report, there was a significant effect of energy dose and longer curing time on the hardness and bond strength with the use of silorane composite resins, which was not manifest for the methacrylate-based composite resins, irrespective of the curing depth.35,38
It has been reported that the shrinkage stresses of a material depend on its elastic modulus. The stresses at interfacial areas during the setting shrinkage of a composite resin are positively correlated with the rigidity of the material based on in vitro studies.39 The elastic modulus, rigidity and mechanical properties of polymers are associated with cross-linking density of the polymer network and the total conversion rate.40 Yamasaki et al41 demonstrated that FS exhibited the highest cross-link density, probably due to the presence of di- and tetra-functional molecules in its composition, which justifies its high modulus and flexural strength compared to methacrylates, as reported by Weinmann et al.15 This agrees with the results observed in this study, in which FS containing multifunctional monomers with the highest cross-link density and greater rigidity and less flexibility due to its higher elastic modulus showed greater gaps in its interface.
In addition, in the current study, two different types of light-cuing units, i.e. LED and QTH, were used for polymerization of composite resin samples. These types of light-curing units were selected due to their popularity and more widespread use by clinicians compared to other light-curing units. However, no differences were observed in gap formation with the use of composite resins polymerized in a similar manner with the use of different types of light-curing units, which coincides with the results of some previous studies.42,43 Similarly, Lee et al44 showed that the amount of polymerization shrinkage is a factor of the type and composition of composite resin, rather than the type of light-curing unit.
Zakavi et al45 reported no statistically significant differences in microleakage at enamel margins between LED and QTH light-curing units; however, significant differences were detected at dentin margins, with LED units exhibiting better performance at dentin margins, which was attributed to the higher consistency between the radiation spectrum of LED units and the absorption spectrum of camphorquinone which is the photoinitiator in conventional composite resins. In contrast, Casseli et al46 showed that the type of the light-curing unit affected gap formation at both the enamel and dentin interfacial areas. The differences might be attributed to differences in adhesive systems and composites used.
Another important result of this study was the fact that the mean gap sizes with the use of both composite resins were smaller at enamel margins in comparison to dentinal margins, consistent with the results of similar previous studies.45,47,48 Since enamel has a homogeneous structure, bonding to enamel is reliable and is achieved with ease; however, it is much more difficult to achieve a favorable bond with dentin, which is attributed to factors such as the non-homogeneous structure of dentin, flow of the dentinal tubular fluid toward the external surface and lower mineral content of dentin compared to enamel.49 Previous studies have reported similar findings with the use of different types of composite resins, including conventional,50 packable50 and nano and silorane composite resins.48
Under the limitations of this in vitro study, with no use of different types of composite resins and curing techniques, it is suggested that in future studies, gaps be measured under a scanning electron microscope (SEM), different bulk-fill composite resins, and other light-curing techniques, including soft start and ramped curing modes.
Conclusion
It was concluded under the limitations of this study that:
-
The type of the light-curing unit did not affect gap formation.
-
The type of the composite resin affected gap formation, with smaller gaps with the use of X-tra Fil composite resin compared to the silorane-base composite resin.
-
There were smaller gaps at enamel margins compared to dentinal margins, irrespective of the type of light-curing unit and the type of the composite resin used.
Acknowledgement
The authors extend their appreciation to the Office of the Vice Chancellor for Research and Dental and Periodontal Research Center Tabriz University of Medical Sciences, for the financial support of this research. This article was derived from an MSc degree thesis in operative dentistry (No.210/T) in Tabriz Faculty of Dentistry. Furthermore, the authors kindly appreciate Dr Morteza Ghojazade for statistical analysis of data and Dr Majid Abdolrahimi for translation of the article into English.
Authors’ contributions
This study was planned by SSO and MB. The literature review was performed by MB, SSO, EJN and AAA. NG and ASO performed the experiments. The statistical analyses and interpretation of data were carried out by ENJ and AAA. MB and NG and ASO drafted the manuscript. All the authors critically revised the manuscript for intellectual content. All the authors have read and approved the final manuscript.
Funding
The authors would like to thank the Office of the Vice Chancellor for Research and Dental and Periodontal Research Center, Tabriz University of Medical Sciences, for the financial support of this study.
Competing interests
The authors declare no competing interests with regards to the authorship and/or publication of this article.
Ethics approval
The study protocol was approved by the Research Ethics Committee of Tabriz University of Medical Sciences.
References
- Pitel ML. Low-Shrink Composite Resins: A Review of Their History, Strategies for Managing Shrinkage, and Clinical Significance. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995) 2013; 34: 578-90.
- Dhingra V, Taneja S, Kumar M, Kumari M. Influence of Fiber Inserts, Type of Composite, and Gingival Margin Location on the Microleakage in Class II Resin Composite Restorations. Operative dentistry 2014; 39: E9-E15.
- Shafiei F, Akbarian S. Microleakage of nanofilled resin-modified glass-ionomer/silorane-or methacrylate-based composite sandwich Class II restoration: effect of simultaneous bonding. Operative dentistry 2014; 39: E22-E30.
- El-Damanhoury H, Platt J. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Operative dentistry 2014; 39: 374-82.
- Braga RR, Ballester RY, Ferracane JL. Factors involved in the development of polymerization shrinkage stress in resin-composites: a systematic review. Dent Mater 2005; 21: 962-70. doi: 10.1016/j.dental.2005.04.018. [Crossref]
- Braga RR, Boaro LC, Kuroe T, Azevedo CL, Singer JM. Influence of cavity dimensions and their derivatives (volume and 'C' factor) on shrinkage stress development and microleakage of composite restorations. Dent Mater 2006; 22: 818-23. doi: 10.1016/j.dental.2005.11.010. [Crossref]
- Witzel MF, Calheiros FC, Goncalves F, Kawano Y, Braga RR. Influence of photoactivation method on conversion, mechanical properties, degradation in ethanol and contraction stress of resin-based materials. J Dent 2005; 33: 773-9. doi: 10.1016/j.jdent.2005.02.005. [Crossref]
- Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc 2003; 134: 1382-90.
- Tiba A, Zeller GG, Estrich CG, Hong A. Laboratory evaluation of bulk-fill versus traditional multi-increment-fill resin-based composites. ADA Professional Product Review 2013; 8: 13-7.
- Guggenberger R, Weinmann W. Exploring beyond methacrylates. Am J Dent 2000; 13: 82d-4d.
- Buergers R, Schneider-Brachert W, Hahnel S, Rosentritt M, Handel G. Streptococcal adhesion to novel low-shrink silorane-based restorative. dental materials 2009; 25: 269-75.
- Mine A, De Munck J, Van Ende A, Cardoso MV, Kuboki T, Yoshida Y, et al. TEM characterization of a silorane composite bonded to enamel/dentin. dental materials 2010; 26: 524-32.
- Ferracane JL. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent Mater 2005; 21: 36-42. doi: 10.1016/j.dental.2004.10.004. [Crossref]
- Rüttermann S, Wandrey C, Raab WHM, Janda R. Novel nano-particles as fillers for an experimental resin-based restorative material. Acta Biomaterialia 2008; 4: 1846-53. doi: doi: 10.1016/j.actbio.2008.06.006.
- Weinmann W, Thalacker C, Guggenberger R. Siloranes in dental composites. Dent Mater 2005; 21: 68-74. doi: 10.1016/j.dental.2004.10.007. [Crossref]
- Pahlavan A, Hasani Tabatabaei M, Arami S, Ataie M, Valizadeh S. Comparison of Polymerization Shrinkage in Methacrylate and Silorane-Based Composites Cured by different LEDs. Journal of Dental Medicine 2013; 26: 27-32.
- Tezvergil-Mutluay A, Lassila L, Vallittu P. Incremental layers bonding of silorane composite: the initial bonding properties. journal of dentistry 2008; 36: 560-3.
- Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Operative Dentistry 2013; 38: 618-25.
- Palin WM, Fleming GJ, Nathwani H, Burke FJ, Randall RC. In vitro cuspal deflection and microleakage of maxillary premolars restored with novel low-shrink dental composites. Dent Mater 2005; 21: 324-35. doi: 10.1016/j.dental.2004.05.005. [Crossref]
- Yamazaki PC, Bedran-Russo AK, Pereira PN, Wsift EJ, Jr. Microleakage evaluation of a new low-shrinkage composite restorative material. Oper Dent 2006; 31: 670-6. doi: 10.2341/05-129. [Crossref]
- Al-Boni R, Raja OM. Microleakage evaluation of silorane based composite versus methacrylate based composite. J Conserv Dent 2010; 13: 152-5. doi: 10.4103/0972-0707.71649. [Crossref]
- Heintze S, Monreal D, Peschke A. Marginal Quality of Class II Composite Restorations Placed in Bulk Compared to an Incremental Technique: Evaluation with SEM and Stereomicroscope. The journal of adhesive dentistry 2015; 17: 147-54.
- Eick JD, Welch FH. Polymerization shrinkage of posterior composite resins and its possible influence on postoperative sensitivity. Quintessence international (Berlin, Germany: 1985) 1986; 17: 103-11.
- Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 2012; 40: 500-5. doi: 10.1016/j.jdent.2012.02.015. [Crossref]
- Lazarchik DA, Hammond BD, Sikes CL, Looney SW, Rueggeberg FA. Hardness comparison of bulk-filled/transtooth and incremental-filled/occlusally irradiated composite resins. The Journal of prosthetic dentistry 2007; 98: 129-40.
- Price R, Murphy DG, Dérand T. Light energy transmission through cured resin composite and human dentin. Quintessence international (Berlin, Germany: 1985) 2000; 31: 659-67.
- Oskoee PA, Kimyai S, Ebrahimi M, Rikhtegaran S, Pournaghi-Azar F. Cervical margin integrity of Class II resin composite restorations in laser-and bur-prepared cavities using three different adhesive systems. Operative dentistry 2012; 37: 316-23.
- Taylor M, Lynch E. Microleakage. Journal of Dentistry 1992; 20: 3-10.
- Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. The journal of adhesive dentistry 2006; 9: 77-106.
- Van Ende A, De Munck J, Van Landuyt K, Van Meerbeek B. Effect of Bulk-filling on the Bonding Efficacy in Occlusal Class I Cavities. J Adhes Dent 2016; 18: 119-24. doi: 10.3290/j.jad.a35905. [Crossref]
- Davidson CL, de Gee AJ. Relaxation of polymerization contraction stresses by flow in dental composites. J Dent Res 1984; 63: 146-8.
- Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR technology. Dent Mater 2011; 27: 348-55. doi: 10.1016/j.dental.2010.11.014. [Crossref]
- Feilzer AJ, de Gee AJ, Davidson CL. Setting stresses in composites for two different curing modes. Dent Mater 1993; 9: 2-5.
- Bouillaguet S, Gamba J, Forchelet J, Krejci I, Wataha JC. Dynamics of composite polymerization mediates the development of cuspal strain. Dent Mater 2006; 22: 896-902. doi: 10.1016/j.dental.2005.11.017. [Crossref]
- Van Ende A, Mine A, De Munck J, Poitevin A, Van Meerbeek B. Bonding of low-shrinking composites in high C-factor cavities. J Dent 2012; 40: 295-303. doi: 10.1016/j.jdent.2012.01.004. [Crossref]
- Hahnel S, Henrich A, Burgers R, Handel G, Rosentritt M. Investigation of mechanical properties of modern dental composites after artificial aging for one year. Oper Dent 2010; 35: 412-9. doi: 10.2341/09-337-l. [Crossref]
- Guiraldo RD, Consani S, Consani RL, Berger SB, Mendes WB, Sinhoreti MA, et al. Comparison of silorane and methacrylate-based composite resins on the curing light transmission. Braz Dent J 2010; 21: 538-42.
- D'Alpino PH, Bechtold J, dos Santos PJ, Alonso RC, Di Hipolito V, Silikas N, et al. Methacrylate- and silorane-based composite restorations: hardness, depth of cure and interfacial gap formation as a function of the energy dose. Dent Mater 2011; 27: 1162-9. doi: 10.1016/j.dental.2011.08.397. [Crossref]
- Feilzer AJ, de Gee AJ, Davidson CL. Relaxation of polymerization contraction shear stress by hygroscopic expansion. J Dent Res 1990; 69: 36-9.
- Sakaguchi RL, Shah NC, Lim BS, Ferracane JL, Borgersen SE. Dynamic mechanical analysis of storage modulus development in light-activated polymer matrix composites. Dent Mater 2002; 18: 197-202.
- Yamasaki LC, De Vito Moraes AG, Barros M, Lewis S, Francci C, Stansbury JW, et al. Polymerization development of "low-shrink" resin composites: Reaction kinetics, polymerization stress and quality of network. Dent Mater 2013; 29: e169-79. doi: 10.1016/j.dental.2013.04.021. [Crossref]
- Cavalcante L, Peris A, Silikas N, Pimenta L. Effect of Light Curing Units on Marginal Adaptation and Hardness of Class II Composite Resin Restorations. J Contemp Dent Pract 2007; 038-45.
- Chandurkar AM, Metgud SS, Yakub SS, Kalburge VJ, Biradar BC. Comparative Evaluation of the Effects of Light Intensities and Curing Cycles of QTH, and LED Lights on Microleakage of Class V Composite Restorations. Journal of clinical and diagnostic research: JCDR 2014; 8: 221.
- Lee S-K, Kim T-W, Son S-A, Park J-K, Kim J-H, KIM H-I, et al. Influence of light-curing units on the polymerization of low-shrinkage composite resins. Dental materials journal 2013; 32: 688-94.
- Zakavi F, Hagh LG, Sadeghian S, Freckelton V, Daraeighadikolaei A, Ghanatir E, et al. Evaluation of microleakage of class II dental composite resin restorations cured with LED or QTH dental curing light; Blind, Cluster Randomized, In vitro cross sectional study. BMC research notes 2014; 7: 416.
- Maia-Casseli DS, Faria-e-Silva AL, Cavalcanti AN, Romani EA, Martins LR. Effect of light-curing unit and adhesive system on marginal adaptation of class v composite restorations. Acta Odontol Latinoam 2012; 25: 68-73.
- Araujo FdO, Vieira L, Monteiro S. Influence of resin composite shade and location of the gingival margin on the microleakage of posterior restorations. Operative dentistry 2006; 31: 556-61.
- Ozel E, Korkmaz Y, Attar N. Influence of location of the gingival margin on the microleakage and internal voids of nanocomposites. J Contemp Dent Pract 2008; 9: 65-72.
- Hassani Tabatabaei M, Ataei M, Safar Charati H. Effects of different curing methods and microleakage and degree of conversion of composite resin restorations. Journal of Dental Medicine 2003; 16: 18-27.
- Tredwin C, Stokes A, Moles D. Influence of flowable liner and margin location on microleakage of conventional and packable class II resin composites. Oper Dent 2005; 30: 32-8.