J Dent Res Dent Clin Dent Prospects. 17(2):71-80.
doi: 10.34172/joddd.2023.36989
Review Article
Assessment of the outcomes and stability after mandibular incisor extraction in orthodontic patients: A systematic review and meta-analysis
Rasiga Gandhi Conceptualization, Investigation, Project administration, Validation, Writing – review & editing, 1, * 
Poornima Jnaneshwar Conceptualization, Supervision, Writing – review & editing, 1 
Keerthi Venkatesan Methodology, Writing – review & editing, 2 
Davis Devasahayam Formal analysis, Methodology, 1 
Krishnaraj Rajaram Data curation, 1 
Rajia Mohamed Azharudeen Data curation, Writing – original draft, 3
Kavichithraa Jothy Investigation, Validation, 4 
Author information:
1Department of Orthodontics and Dentofacial Orthopaedics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India
2Department of Orthodontics and Dentofacial Orthopaedics, Faculty of Dental sciences, SRIHER, Chennai, Tamilnadu, India
3Orthodontist, Private Practice, Kadayanallur, Tenkasi, Tamilnadu, India
4Department of Orthodontics, Adhiparasakthi Dental College & Hospital, Melmaruvathur, Chengalpattu, India
Abstract
Background.
This study assessed the stability of the outcomes after mandibular incisor extraction (MIE) using intercanine width and peer assessment rating (PAR) scores in orthodontic patients.
Methods.
PubMed, Cochrane Library, Science Direct, Google Scholar, Ovid, and SciELO were systematically searched without restrictions until August 2022. A risk of bias assessment was performed using Newcastle-Ottawa Scale (NOS). The Grading of Recommendations, Assessment, Development, and Evaluation tool was used to assess the quality of evidence. Random effects meta-analysis was performed using RevMan software.
Results.
Seven retrospective studies met the inclusion criteria and were included. Meta-analysis identified a statistically significant reduction in intercanine width with MIE after the retention period. The mean difference in post-retention changes concerning intercanine width (MD=0.14, 95% CI: -2.17–1.89; P<0.00001) was significantly higher in premolar extraction (PE) compared to incisor extraction and significantly less in non-extraction compared to incisor extraction (MD=0.72, 95% CI: -0.59–2.03; P<0.00001). Improvements in PAR scores from the start of treatment to the retention period indicated a high outcome standard (>70%) with MIE treatment, with no significant difference in the reduction percentage compared to premolar and non-extraction groups.
Conclusion.
With the existing retrospective studies of limited evidence, treatment outcomes with MIE were found to show good improvements in PAR scores. Some reduction in the intercanine width was evident after the retention period, which was observed even with the other two treatment modalities that were compared. Hence, with careful evaluation, MIE could be considered a valid treatment option.
Keywords: Intercanine width, Mandibular incisor extraction, Orthodontic patients, PAR index, Relapse, Stability
Copyright and License Information
©2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Introduction
The debate of extraction versus non-extraction approach in orthodontic treatment has always been long-standing. The treatment trends were observed to fluctuate between non-extraction and extraction of four premolars.1 Mandibular incisor extraction (MIE) has been reported as a rare extraction choice in orthodontic treatment with a frequency ranging from 2.1%2 to 6%.3
The concept was first proposed by Hahn,4 and extraction of single or even two incisors was presented in literature predominantly as case reports and case series. Kokich and Shapiro recommended that with careful planning, case selection, and a complete diagnostic setup, intentional extraction of lower incisors can lead to good results with minimal orthodontic manipulation.5 The following indications have been strongly recommended for MIE: class I molar relationship, moderate crowding in mandibular anterior teeth, mild or no crowding in the maxillary anterior teeth, acceptable soft tissue profile, minimal to moderate overjet and overbite, minimal growth potential and tooth size discrepancies (peg laterals, missing laterals).6,7 It has been suggested as a good treatment alternative in mild to moderate class III malocclusion with reduced overjet and overbite.8
Many authors object to the treatment plan of incisor extraction, citing unwanted treatment effects, including non-coincidental midlines,9 increased overjet and overbite, mesial tipping of canine, which can cause difficulties in achieving class I canine relationship, lingually tipped incisors, inadequate space, excess space creation and space reopening,10 relapse of crowding of the incisors,11 unfavorable posterior occlusion,12 loss of interdental papillae, and appearance of less aesthetic black triangles.13 This led to the description of MIE as a compromised treatment approach. However, some authors considered it an ‘acceptable compromise’ and a valid treatment option though ideal occlusion standards were not met.14 MIE has been advocated in orthodontic practice with fixed appliances to date and has also been carried out with Invisalign treatment.15
Although the treatment looks successful from the above-discussed perspective, actual treatment success lies in the stability of achieved results. The view on stability appears controversial as contradictory statements were found, with some reporting stable results,7,16-18 while others reported instability and promoted the need for long-term retention.19 The presence of lingually bonded retainers resulted in less relapse than in patients without a retainer.20
Valinoti reported that lower incisor extraction is less likely to exhibit relapse after retention based on factors such as i) proximity of incisor to crowding, requiring minimal tooth movement, and preserving larger areas of the original position of teeth; ii) less load on anchor teeth during space closure utilizing most space for anterior correction; iii) muscle pressure does not establish instability with minimal interaction of tongue and lips on unaltered tooth position.16 Maintenance or minor change in intercanine width has also been reported.17 Existing systematic reviews on MIE were overall reviews21-23 or comparisons have been made with interproximal reduction.24 This systematic review assessed the stability of treatment results analyzed by considering parameters like intercanine width and peer assessment rating (PAR) scores after MIE in orthodontic patients.
Methods
Protocol and registration
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) protocolwas followed, and the systematic review was registered with PROSPERO (CRD42020196379).
Eligibility criteria
Studies fulfilling the following criteria were included:
-
Participants: Orthodontic patients evaluated during the retention period
-
Interventions: Orthodontic treatment with MIE
-
Comparisons: Patients treated orthodontically with all four premolar extractions (PE) or non-extraction (NE)
-
Primary Outcome: Changes in intercanine width
-
Secondary outcome: PAR index scores
-
Study design: Longitudinal studies, either prospective or retrospective
The exclusion criteria were studies without a control group, case reports, case series with no statistical analysis, reviews, expert opinions, and letters to the editor.
Data sources
PubMed, Cochrane Library, Science Direct, Google Scholar, Ovid, and SciELO were systematically searched without restrictions in the year of publication or language up to August 2022.
Search strategy
The search strategy followed for the six search engines is presented in Table 1.
Table 1.
Search strategy followed in different databases
|
Search engines
|
|
| PubMed |
(incisor extraction[Title/Abstract]) AND (intercanine width[Title/Abstract] OR stability[Title/Abstract] OR PAR index[Title/Abstract] OR irregularity[Title/Abstract] OR relapse[Title/Abstract] OR outcome*[Title/Abstract] OR Peer Assessment Rating[Title/Abstract]) |
| Cochrane |
(mandibular incisor extraction) AND (intercanine width) OR (post-orthodontic stability) |
| Google Scholar |
"Mandibular incisor extraction" and changes in intercanine width or post-treatment stability in orthodontic patients |
| SciELO |
(ab:(incisor extraction AND intercanine width)) OR (ab:(incisor extraction AND stability)) OR (ab:(incisor extraction AND PAR index)) OR (ab:(incisor extraction AND irregularity)) OR (ab:(incisor extraction AND relapse)) OR (ab:(incisor extraction AND outcome)) OR (ab:(incisor extraction AND outcomes)) OR (ab:(incisor extraction AND Peer Assessment Rating)) |
| Science Direct |
Mandibular incisor extraction, changes in intercanine width, or post-orthodontic stability |
| Ovid |
((intercanine width or stability or irregularity or relapse or outcome or Peer Assessment Rating) and incisor extraction) |
| Web of Science |
ALL = (“incisor extraction”) AND ALL = (intercanine width OR stability OR PAR index OR irregularity OR relapse OR outcome OR outcomes OR Peer Assessment Rating) |
Study selection
The titles and abstract results were screened, and irrelevant articles and duplicates were excluded. Three reviewers independently assessed the articles for eligibility and obtained full texts. References were hand-searched for additional relevant studies. Finally, articles that met the above inclusion criteria were selected.
Data collection and data items
Three reviewers independently collected data using a data collection form with a standardized table. All linear measurements and percentage scores measured before treatment, after treatment, and after the retention period were extracted. The data were compared for accuracy, and any conflicts were resolved by reexamining the original study and discussions between the reviewers until a consensus was achieved.
Assessment of bias risk within studies
The risk of bias in nonrandomized studies was assessed using a modified version of the Newcastle-Ottawa Scale (NOS).25 The reviewers used a star system and assessed eight domains and three criteria, patient selection (maximum of four points), comparability (two points), and assessment of outcome (three points for exposure/outcome), and then the overall bias was judged. Four stars or less indicated low quality or high ROB, 5‒6 stars indicated moderate ROB, and > 7 indicated low ROB.
Evaluation of the level of evidence
The level of evidence was assessed using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) (https://gradepro.org/).26 For each outcome examined, the GRADE assesses the number of studies included, the studies’ designs, risk of bias, inconsistency, indirectness, imprecision, and other considerations (such as publication bias). Depending on the seriousness of the limitation in each one of these domains, the evidence could be downgraded by 1 or 2 levels. Based on this assessment, the certainty of evaluating the outcome could be very low, low, moderate, or high quality.
Summary measures
The outcome measures were differences in means of the intercanine width (mm) and the percentages of mean reduction in PAR scores. Meta-analysis was performed using Review Manager (RevMan) version 5.4 (The Nordic Cochrane Centre, Copenhagen, Denmark).
Synthesis of results
The data extracted were descriptively tabulated. Meta-analysis results were graphically represented with forest plots. Clinical heterogeneity was assessed by comparing the study design, control groups, and methodologies. Statistical heterogeneity was evaluated with the Cochrane Tau2, χ2 and I2 statistics (low = 25%, moderate = 50%, and high = 75%). Studies were statistically evaluated, and significance was established at P < 0.05. I2 with a 95% confidence interval (CI) and the P value for χ2 were interpreted together. Random effects meta-analysis was carried out when there were high levels of clinical or statistical heterogeneity.
Results
Study selection
The search yielded no results of randomized control trials or prospective studies; all the included studies were nonrandomized retrospective studies. The search strategy yielded 453 studies from electronic databases and hand searches. Removing duplicates and applying eligibility criteria resulted in 20 articles for full-text evaluation. Seven articles were included in this systematic review and subjected to data collection and quantitative synthesis.18-32 The complete search strategy and reasons for exclusion after full-text assessment are provided in the PRISMA flowchart (Figure 1).
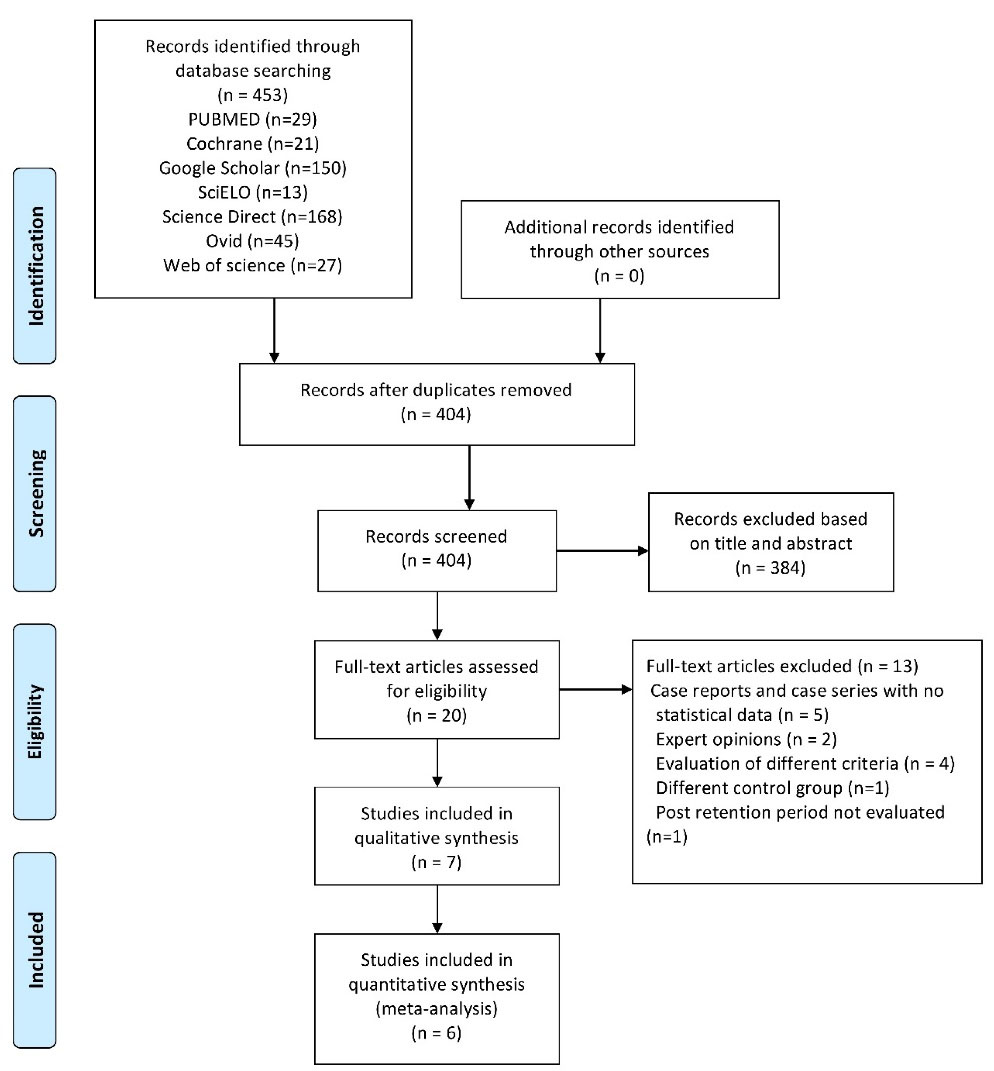
Figure 1.
PRISMA flowchart of article retrieval.
.
PRISMA flowchart of article retrieval.
Study characteristics
Table 2provides descriptive characteristics of the studies included. Eighty-four individuals had undergone single incisor extraction in three studies, with intercanine width as one of the parameters evaluated18,27,28 and 100 individuals in the studies evaluating the PAR index.29-32 The participants were adults with an age range of 18‒35 years, treated with fixed appliances. Malocclusion involved was predominantly class I, and two studies evaluated class II and class I malocclusion.18,29 Post-retention follow-up varied vastly from 3 to 12 years among studies assessing intercanine width.18,27,28 Riedel et al18 used a removable retainer worn for two years,and Mahmoudzadeh et al27 used a clear or Hawley’s retainer. The patients were evaluated after 3.5 years,and all the patients had lingually bonded retainers for one year in the study by Verma and Jain et al.28 PAR scores were evaluated before and after treatment with no post-retention follow-up and no information on retention protocol.29-32
Table 2.
Summary of the study characteristics of the included studies
|
Studies
|
Study design
|
Participants
|
Intervention
|
Control
|
Outcome
|
Riedel et al,
199218 |
Retrospective study |
107 Patients |
42 patients
24 patients – single mandibular incisor extraction group
18 patients – two mandibular incisor extraction group
(15 males, 27 females)
mean age: 35.3 (24.10-57.8) years |
65 previously reported PE cases
(24 males, 41 females)
mean age 30.1 (25-43.4) years |
Intercanine width decreased during treatment and continued to decrease post-retention in most cases.
(statistically significant)
More stable than PE cases. |
| Mahmoudzadeh et al, 201827 |
Retrospective study |
120 Patients |
40 patients in MIE group
(31 females, 9 males)
mean age: 21.6 ± 4 years |
NE group: 40 patients
(33 females, 7 males) mean age: 24 ± 6 years |
Intercanine width decreased during treatment and continued to decrease post-retention in the MIE group. There was not much difference in the intercanine width in the NE and PE groups.
There was no significant difference among the means in the three study groups. |
PE group: 40 patients
(35 females, 5 males)
mean age: 22.9 ± 5 years |
| Verma and Jain, 202228 |
Retrospective study |
32 Patients |
Lower incisor extraction protocol (n= 17) |
NE protocol (n= 15) |
Intercanine width increased significantly in the NE group post-treatment, and there was a significant relapse during post-retention follow-up. Overall the intercanine width reduced or remained unchanged in the incisor extraction group. |
| Ileri et al, 201229 |
Retrospective study |
60 Subjects |
Extraction of a lower incisor group (MIE)
20 patients (13 females and 7 males) |
Extraction of four first premolars group (PE)
20 patients (13 females and 7 males) |
The percentage PAR reduction was lesser than in other groups. Orthodontic treatment without extraction had a better treatment outcome than the four-first PE and single lower incisor extraction protocols in Class I cases with moderate to severe mandibular anterior crowding. |
NE group
20 patients (13 females and 7 males) |
| Kamal et al, 201730 |
Retrospective study |
108 Patients |
MIE group
36 patients
Age: 19.0 ± 2.3 years. |
NE group, 36 patients
Age: 18.9 ± 4.1 years |
Differences between NE and MIE groups, and PE and MIE groups were statistically significant.
Difference between NE and PE (not statistically significant)
Percentages of improvement in PAR scores showed no significant difference among patients treated with NE, PE, and MIE.
Mean improvements in the maxillary and mandibular anterior segment were greater in the MIE group. |
PE group, 36 patients
Age: 19.2 ± 3.6 years |
| Lee et al, 201931 |
Retrospective study |
28 Patients |
MIE cases (n = 14) |
NE controls (n = 14) |
There were no significant differences in the treatment outcomes of orthodontic cases treated with MIE or NE. |
| Maaz et al, 202232 |
Cross-sectional study |
90 Patients |
MIE cases (n = 30)
Mean age: 20.21 ± 3.00 years |
NE cases (n = 30)
Mean age: 20.52 ± 4.08 years |
There were significant differences in the percentage improvement for the PAR (P = 0.010) NE, PE, and MIE showing median percentage improvements of 82.1%, 91.3%, and 74.1%, respectively. |
PE cases (n = 30)
Mean age: 20.42 ± 3.46 years |
PAR, peer assessment rating; PE, premolar extraction; MIE, mandibular incisor extraction; NE, non-extraction.
Risk of bias within studies
Table 3 presents the risk of bias for each study. Riedel et al18 compared intercanine width in the post-retention period of patients who underwent lower incisor extraction. Data from previous research showed that this lack of a control group from a similar population and time led to a high risk of bias. The overall assessment showed a low risk of bias in four of the seven studies,28,30-32 and two studies had a moderate risk of bias.27,29
Table 3.
Newcastle Ottawa Scale for observational studies
|
Studies
|
Selection
(maximum 4 stars)
|
Comparability
(maximum 2 stars)
|
Outcome (maximum 3 stars)
|
Total stars (9)
|
Risk of bias
|
| Retrospective studies |
Representativeness of the exposed cohorts |
Selection of the non-exposed cohort |
Ascertainment of exposure |
Justification of study sample size |
Comparability of cohorts on the basis of design or analysis |
Assessment of outcome |
Was follow-up long enough for the outcome to occur |
Adequacy of follow-up of cohorts |
|
|
|
|
a) Truly representative of the average in the target population* (all subjects or random sampling);
b) Somewhat representative of the average in the target population* (nonrandom sampling);
c) Selected group of patients;
d) No description of the sampling strategy. |
a) drawn from the same community as the target population*;
b) drawn from a different source.
c) no description of the derivation of the comparison population. |
a) Secure records (e.g., surgical records)*
b) Structured interview*
c) Written self-report
d) no description |
a) Yes*
b) No |
The subjects in different outcome groups are comparable based on the study design or analysis. Confounding factors are controlled.
a) The study controls for
age and type of malocclusion*;
b) The study controls for retention.*
c) Study does not control for any of the above |
a) Independent blind assessment*;
b) Record linkage*;
c) Self-report;
d) No description. |
a) Yes-after completion of orthodontic treatment*
b) No |
a) Complete follow-up - all subjects accounted for*
b) Subjects lost to follow-up unlikely to introduce bias - small number lost (follow up, or description provided of those lost)*
c) Follow-up rate and no description of those lost
d) No statement |
|
|
Riedel et al,
199218 |
c |
b |
a* |
b |
c |
b* |
a* |
b* |
4 |
High |
| Mahmoudzadehet al, 201827 |
c |
a* |
b* |
a* |
b* |
b* |
a* |
c |
6 |
Moderate |
| Verma and Jain, 202228 |
c |
a* |
a* |
a* |
a*,b* |
b* |
a* |
b* |
8 |
Low |
| Cross sectional studies |
Representativeness of the exposed cohorts |
Selection of the non-exposed cohort |
Ascertainment of exposure |
Justification of study sample size |
Comparability of cohorts on basis of design or analysis |
Assessment of outcome |
Same method of ascertainment for exposed and non-exposed group |
Statistical test |
|
|
|
|
a) Truly representative of the average in the target population* (all subjects or random sampling);
b) Somewhat representative of the average in the target population* (nonrandom sampling);
c) Selected group of patients;
d) No description of the sampling strategy. |
a) Drawn from the same community as the target population*;
b) Drawn from a different source.
c) No description of the derivation of the comparison population. |
a) secure record (e.g. surgical records) *
b) structured interview *
c) written self-report
d) no description |
a) Justified and satisfactory. *
b) Not justified. |
The subjects in different outcome groups are comparable, based on the study design or analysis. Confounding factors are controlled.
a) The study controls for
age, sex*;
b) Type of malocclusion.*
c) Study does not control for any of the above |
a) Independent blind assessment*;
b) Record linkage*;
c) Self-report;
d) No description. |
a) Yes*
b) No |
a) The statistical test used to analyze the data is clearly described and appropriate, and the measurement of the association is presented, including confidence intervals and the probability level (p value).*
b) The statistical test is not appropriate, not described or incomplete. |
|
|
| Ileri et al, 201229 |
c |
a* |
a* |
b |
a* |
b* |
a* |
a* |
6 |
Moderate |
| Kamal et al,201730 |
c |
a* |
a* |
a* |
a*,b* |
b* |
a* |
a* |
8 |
Low |
| Lee et al, 201931 |
c |
a* |
a* |
a* |
a*,b* |
b* |
a* |
a* |
8 |
Low |
| Maaz et al 202232 |
c |
a* |
a* |
a* |
a*,b* |
b* |
a* |
a* |
8 |
Low |
Synthesis of results
Results of individual studies and meta-analysis
Table 4 summarizes the results of variables assessed in the studies.
Table 4.
Results of the individual studies
|
Changes in intercanine width
|
|
Studies
|
Malocclusion treated
|
Treatment duration
|
Intercanine width
|
Difference
|
Significance of difference
P
value
|
Riedel et al,
199218 |
Class I
Class II div 1
Class II div 2 |
Post-retention period:
12.9 years (6.6-24) |
Single incisor extraction cases:
Pre-treatment: 24.37 ± 2.53 mm
Post-treatment: 22.77 ± 1.10 mm
Post-retention: 21.64 ± 1.41 mm |
D1
-1.63 ± 2.22 mm
D2
-1.13 ± 0.95 mm |
P0.05*
D1 and D2 |
|
|
PE1: scatter diagram of intercanine width |
D2
-2.02 ± 1.57 mm |
P < 0.0001*** |
| Mahmoudzadeh et al, 201827 |
Class I or Class II Division 1 malocclusion |
Retention period: 8 months ± 4.7
Post-retention period: 3.35 ± 1.48 years |
MIE cases:
Pre-treatment: 25.56 ± 2.19 mm
Post-treatment: 23.02 ± 2.02 mm
Post-retention: 22.37 ± 1.24 mm |
D2
-0.65 ± 1.58 mm |
P = 0.012 * |
NE cases:
Pre-treatment: 26.30 ± 1.58 mm
Post-treatment: 26.61 ± 1.79 mm
Post-retention: 25.94 ± 1.61 mm |
D2
-0.67 ± 1.18 mm |
P = 0.001* |
PE cases:
Pre-treatment: 26.82 ± 2.51 mm
Post-treatment: 26.80 ± 1.56 mm
Post-retention: 26.27 ± 1.85 mm |
D2
-0.53 ± 1.14 mm |
P = 0.006* |
|
Between groups P = 0.870 NS |
| Verma and Jain, 202228 |
Class I malocclusion |
Post-retention period: 1 year after completion of treatment |
MIE cases:
Pre-treatment: 23.5 ± 1.7 mm |
D1
-0.94 ± 0.35 mm
D2
-0.01 ± 0.05 mm
D3
-0.95 ± 0.47 mm |
P < 0.05 * |
NE cases:
Pre-treatment: 22.8 ± 2.9 mm |
D1
2.01 ± 0.18 mm
D2
-1.37 ± 0.40 mm
D3
0.65 ± 0.58 mm |
|
Changes in the PAR index scores
|
|
Studies
|
Malocclusion treated
|
Treatment duration
|
PAR Scores
|
PAR improvement 1percentage
|
Significance of difference
P
value
|
| Ileri et al, 201229 |
Class I malocclusion and moderate crowding |
1.6 ± 0.9 years |
MIE cases:
Pre-treatment: 21.5 ± 1.5
Post-treatment: 3.8 ± 3.52 |
80.3 ± 18% |
P < 0.05*
Between groups MIE & NE P = 0.047*, others NS |
| 2 ± 0.4 years |
PE cases:
Pre-treatment: 27 ± 6.2
Post-treatment: 3.5 ± 3.19 |
87.7 ± 10.2% |
| 1.3 ± 0.4 years |
NE cases:
Pre-treatment: 17.1 ± 5.7
Post-treatment: 1.4 ± 1.14 |
91.2 ± 9.2% |
| Kamal et al, 201730 |
Class I malocclusion |
|
MIE cases:
Pre-treatment: 33.3 ± 10.4
Post-treatment: 9.1 ± 7.5 |
70.6 ± 24.1% |
P < 0.001**
Between groups P = 0.351 NS |
PE cases:
Pre-treatment: 23.5 ± 9.4
Post-treatment: 5.5 ± 3.7 |
73.1 ± 19.4% |
NE cases:
Pre-treatment: 20.5 ± 9.5
Post-treatment: 4.7 ± 4.2 |
75.8 ± 25.8% |
| Lee et al, 201931 |
Class I malocclusion or a mild tendency toward Class III, moderate crowding (4–8 mm) in the lower arch |
|
MIE cases:
Pre-treatment: 18.8 ± 7.3
Post-treatment: 3.8 ± 3.1
Changes: 15.0 ± 8.6 |
73.2 ± 32.1% |
Between groups P = 0.874 NS |
NE cases:
Pre-treatment: 16.7 ± 8.4
Post-treatment: 4.0 ± 4.4
Changes: 12.7 ± 8.0 |
75.6 ± 25.2% |
| Maaz et al 202232 |
Class I malocclusion |
|
MIE cases: |
80% |
P = 0.010 *
Between groups MIE & PE P = 0.002*, others NS |
| PE cases: |
98% |
| NE cases: |
89.1% |
PAR, peer assessment rating; PE, premolar extraction; MIE, mandibular incisor extraction; NE, non-extraction.
D1: difference from post-treatment to pre-treatment, D2: difference from post-retention to post-treatment, D3: difference from post-retention to pre-treatment.
Statistically significant at * P < 0.05; **P < 0.001; ***P < 0.0001; NS, No significant.
A reduction in intercanine width during treatment and post-retention was reported in the MIE group.18,27,28 Two studies showed a decrease in intercanine width post-treatment and post-retention.18,27 Among them, one reported intercanine width reduction post-retention in single incisor extraction (1.13 ± 0.95 mm) and two incisor extraction (1.39 ± 1.19 mm).18 Another study by Mahmoudzadeh et al27 reported a post-retention decrease in intercanine width in MIE (0.65 ± 1.5 mm), NE (0.67 ± 1.18 mm) and PE (0.53 ± 1.14 mm).In the study by Vermaet al,28 there was an increase in intercanine width in the NE group, and intercanine width decreased by 0.94 mm in MIE.
When PAR scores were evaluated between pre-treatment and post-treatment periods, they were significantly reduced post-treatment, and percentage improvement was reported.29-32 The mean percentage improvement of PAR reported by Ileri et al29 in MIE was 80.3%, NE was 91.2%, and PE was 87.7%.Kamal et al30 reported percentage improvements of 70.6 ± 24.1% in MIE, 75.8 ± 25.8% in NE and 73.1 ± 19.4% in PE.Lee et al31 reported an improvement of 73% in MIE and 76% in the NE group. Maaz et al32 reported an 80% PAR percentage improvement in MIE, 98% in PE, and 89.1% in NE.
There was relative clinical homogeneity in the assessment methods and reporting the mean changes of the intercanine and PAR scores in the mandibular incisor and PE groups and the NE group in six studies included in the meta-analysis.18,27-31 Forest plot was used to compare the mean difference (MD) in intercanine width changes between the post-treatment and post-retention periods in incisor extraction with PE (Figure 2) and NE (Figure 3) to quantitatively determine whether there was a significant reduction post-retention. A statistically significant decrease in mean intercanine widthwas seen between the premolar and incisor extraction groups (MD = 0.14, 95% CI: -2.17–1.89; P < 0.00001). When the intercanine width changes of the incisor extraction and NE groups were compared, a statistically significant reduction in mean intercanine widthwas evident in the incisor extraction group compared to the NE group (MD = 0.72, 95% CI: -0.59–2.03; P < 0.00001). Both comparisons showed high heterogeneity, and a random effects model was used. Standard random-effects approaches added a common component of variance to each study weight in the presence of heterogeneity to account for the variation in treatment effects between trials, and the relative weights were more balanced than those awarded under fixed effects.33
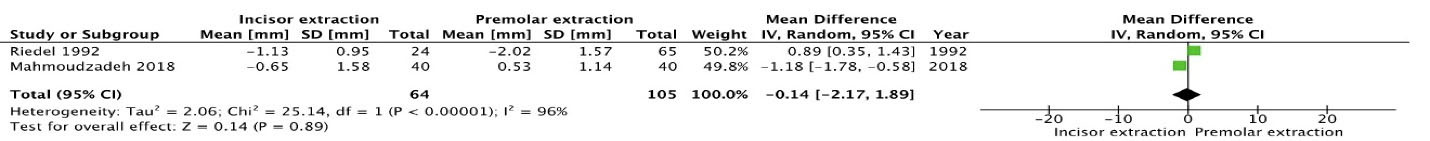
Figure 2.
Forest plot comparing pre-treatment and post-retention intercanine (IC) width reduction in mandibular incisor extraction compared to premolar extraction.
.
Forest plot comparing pre-treatment and post-retention intercanine (IC) width reduction in mandibular incisor extraction compared to premolar extraction.
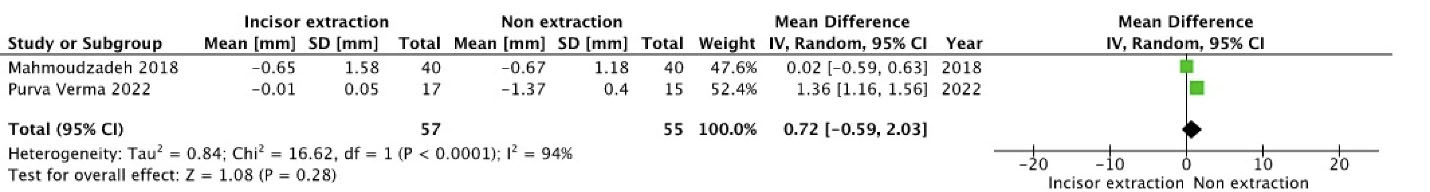
Figure 3.
Forest plot comparing post-treatment and post-retention intercanine (IC) width reduction in mandibular incisor extraction compared to non-extraction.
.
Forest plot comparing post-treatment and post-retention intercanine (IC) width reduction in mandibular incisor extraction compared to non-extraction.
For the clinical relevance of improvement in treatment results, PAR reduction percentages of MIE were compared individually with four PEs (Figure 4) and NE (Figure 5). The mean difference was calculated, and there was no significant differencein PAR reduction percentage between mandibular incisor and four PE groups (MD = -5.21, 95% CI: -11.96–1.53; P = 0.48) or between lower incisor extraction and NE groups (MD = -8.16, 95% CI: -14.84 – -1.49; P = 0.64). The forest plots showed low heterogeneity, with the left side favoring lower incisor extraction and the right side favoring the premolar or NE group.
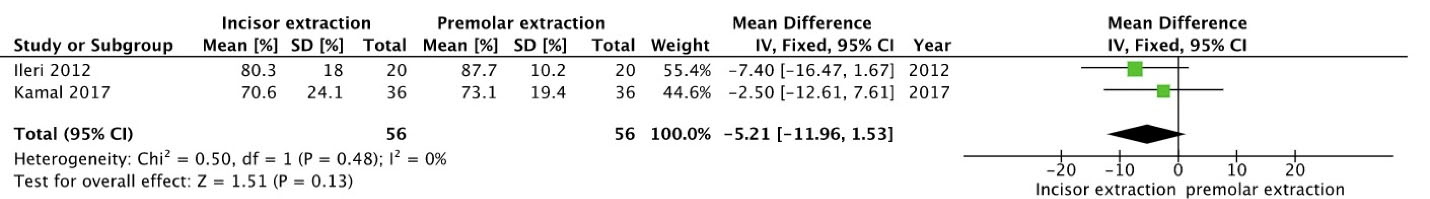
Figure 4.
Forest plot comparing PAR reduction percentages of mandibular incisor extraction and premolar extraction.
.
Forest plot comparing PAR reduction percentages of mandibular incisor extraction and premolar extraction.
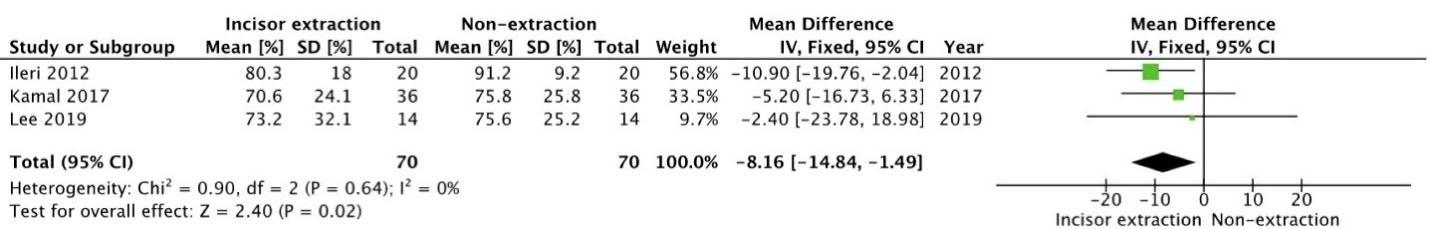
Figure 5.
Forest plot comparing PAR reduction percentages of mandibular incisor extraction and non-extraction.
.
Forest plot comparing PAR reduction percentages of mandibular incisor extraction and non-extraction.
Quality analysis
Table 5 summarizes the quality assessment of outcomes from included articles using GRADE. The overall effect was considered very low certainty for studies evaluating the intercanine width and low for the PAR index. In general, observational studies showed inconsistency in retention methods and follow-up durations. Riedel et al did not have a uniform control group, and they were the main factors for the limited quality of evidence.
Table 5.
GRADE assessment
|
Certainty assessment
|
№ of patients
|
Effect
|
Certainty
|
Importance
|
|
No. of studies
|
Study design
|
Risk of bias
|
Inconsistency
|
Indirectness
|
Imprecision
|
Other considerations
|
Incisor extraction
|
PE or NE
|
Relative
(95% CI)
|
Absolute
(95% CI)
|
|
Intercanine Width (follow-up: range 1 to 10 years)
|
| 3 |
observational studies |
Not serious |
Not serious |
Seriousa |
Not serious |
None |
81 |
160 |
- |
Not estimable |
⨁◯◯◯
Very low |
|
|
PAR Index
|
| 4 |
observational studies |
Not serious |
Not serious |
Not serious |
Not serious |
None |
100 |
186 |
- |
Not estimable |
⨁⨁◯◯
Low |
|
CI, confidence interval; PAR, peer assessment rating; PE, premolar extraction; NE, non-extraction.
Question:Incisor extraction compared to PE or NE in treatment results and stability.
aRiedel study showed serious indirectness in reporting data, and the sample size is heterogeneous.
GRADE Working Group grades of evidence
High certainty: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
Discussion
This systematic review assessed the treatment outcomes and stability in studies where MIE was adopted as a treatment option. On screening the available literature, seven studies met the inclusion criteria of this systematic review. All seven studies were retrospective observational studies and were of very low to low evidence, which was assessed by the GRADE tool. Mandibular intercanine width was one of the outcomes assessed in studies in which MIE was carried out.18,27,28 The stability of treatment was assessed as maintaining dental arch form and arch widthis essential for stable orthodontic treatment results.34 Some studies reported pre-treatment and post-treatment changes in PAR scores as one of the most common tools used in orthodontics to validate treatment outcomes.29-32
Maintaining the intercanine width or minimal alterations post-retention can be considered one key factor for stable results. On observation of treatment changes and post-retention changes, a predominant reduction was found to occur between pre-treatment and post-treatment in MIE(Table 4).This can be attributed to the fact that during treatment with incisor extraction, intercanine width tends to decrease as tooth material reduction occurs upon the removal of the mandibular incisor. Dacre11 studied the untreated cases compared to incisor extraction, and a reduction in intercanine width of 0.3 ± 1.30 mm was observed in the long term, even in the absence of treatment, suggesting a decrease in intercanine width with age.According to Burke et al,35 mandibular intercanine width tends to expand during treatment on the order of 1‒2 mm and contract post-retention to approximately the original dimension, regardless of patient diagnostic and treatment modalities.
Riedelet al18 reported a reduction in both single and two MIE groups and found it significantly less than PE cases with no significant correlation between treatment and post-retention changes. They suggested that it might satisfy the requirements of maintaining arch form without expanding intercanine width, while in PE therapy, an increase in intercanine width might be required to gain alignment. Post-treatment and post-retention evaluations of intercanine width showed some reduction in the evaluated studies.18,27,28 In the meta-analysis, there was a significantly greater reduction in intercanine width in the PE group compared to MIE (Figure 2). Mahmoudzadeh et al27 reported no statistically significant difference in the intercanine width in post-retention changes between incisor extraction, NE, and PE.
According to Vermaet al,28 there was a mild decrease in intercanine width in the incisor extraction group, which was maintained post-retention, whereas, in the NE group, there was an increase in intercanine width that reduced to a greater extent post-retention. When this increase in intercanine distance was analyzed in NE cases, it was noticed that the NE control group was treated by self-ligating brackets, which might be a reason for this increase. Interproximal reduction is sometimes carried out in NE treatment to address Bolton’s discrepancies. A systematic review showed that both interproximal wear and incisor extraction are effective in treating moderate anterior crowding, and one of the studies reviewed reported that the stability of treatment outcomes was evident as there was no change in intercanine width in patients who underwent proximal stripping.24 Similarly, in the present research, a meta-analysis comparing the incisor extraction and NE groups showed a greater reduction in intercanine width in the incisor extraction group(Figure 3).When MIE was compared to PE and NE treatment protocol (Figures 2 and 3), post-retention changes in intercanine width in MIE cases were significantly greater than in NE and less than in PE groups. Extraction of mandibular incisors in selected cases of Bolton excess in the mandibular anterior region to gain space to alleviate crowding is thus justified.
Ileri et al29 reported that the mean improvement in PAR scores was the highest in NE followed by PE and least in the MIE group, and the same results were reported by Maaz et al.32 The least reduction in MIE was thought to be probably due to increasing overjet and overbite. The meta-analysis comparing PAR score improvement percentages of MIE and NE, MIE, and PE showed no significant differences(Figures 4 and 5). These findings were confirmed by Kamal et al30 and Lee et al.31
All the studies assessing PAR scores29 showed > 70% reduction in PAR percentage scores with MIE, which is considered a high standard outcome according to Richmond et al.36 None of the studies assessed PAR post-retention but the PAR index, in general, can be considered an indicator of stability as PAR index follow-up studies have shown good stability up to 76.3%.37
The positive outcomes observed through this systematic review suggest that MIE can be a clinically effective treatment modality in carefully selected cases. Orthodontists should pursue MIE as a valuable option to provide results in cases like class I malocclusion with mild to moderate crowding, mild class III tendency, acceptable soft tissue profile, moderate overjet and overbite, and Bolton’s discrepancies. Negligible relapse in the anterior area, maintenance of soft tissue profile, and no compromise in esthetics or function can be worthwhile results achieved with shorter treatment time and simpler mechanics.
Limitations and Future Directions
All the studies included in this systematic review were retrospective. The paucity of randomized controlled trials proved to be a limitation.
The PAR index is not an optimal tool for evaluating treatment benefits and does not consider all factors important for the total quality of treatment.38 PAR provides only a general impression of dental arches, and no individual dental variables are considered.
As there is a scarcity of studies on the assessment of post-treatment stability, and study designs also greatly vary concerning post-retention stability of intercanine width, drawing a conclusion remains challenging, indicating the need for more studies, controlled trials with matched controls, and similar pre-treatment characteristics and post-retention period. Maintaining records and longer post-retention follow-ups are thus emphasized to provide better long-term studies and evidence.
Conclusion
The retrospective studies in this systematic review provided limited quality evidence, making it difficult to draw significant evidence-based conclusions. More well-designed studies are required for a definitive conclusion on long-term stability. Thus the conclusions derived were as follows:
-
There was a reduction in intercanine width during post-retention, significantly higher in PE than MIE. However, there was significantly less intercanine width reduction in the NE group than in incisor extraction.
-
The high standard of outcome analyzed with PAR scores suggested MIE as a valid treatment option, and the results were comparable with PE and NE groups, with no significant difference between the groups.
-
One treatment option cannot be better than the other, and treatment choices should be made according to the clinical situation.
Competing Interests
The authors declare that they have no competing interests with regard to the authorship and/or publication of this article.
Ethical Approval
Not applicable.
Funding
There were no sources of funding for the study.
References
- Janson G, Maria FR, Bombonatti R. Frequency evaluation of different extraction protocols in orthodontic treatment during 35 years. Prog Orthod 2014; 15(1):51. doi: 10.1186/s40510-014-0051-z [Crossref] [ Google Scholar]
- Weintraub JA, Vig PS, Brown C, Kowalski CJ. The prevalence of orthodontic extractions. Am J Orthod Dentofacial Orthop 1989; 96(6):462-6. doi: 10.1016/0889-5406(89)90112-1 [Crossref] [ Google Scholar]
- Proffit WR. Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthod 1994; 64(6):407-14. doi: 10.1043/0003-3219(1994)064<0407:froefa>2.0.co;2 [Crossref] [ Google Scholar]
- Hahn GW. Problems in the treatment of malocclusion. Angle Orthod 1942; 12(2):61-82. doi: 10.1043/0003-3219(1942)012<0061:pittom>2.0.co;2 [Crossref] [ Google Scholar]
- Kokich VG, Shapiro PA. Lower incisor extraction in orthodontic treatment: four clinical reports. Angle Orthod 1984; 54(2):139-53. doi: 10.1043/0003-3219(1984)054<0139:lieiot>2.0.co;2 [Crossref] [ Google Scholar]
- Owen AH. Single lower incisor extractions. J Clin Orthod 1993; 27(3):153-60. [ Google Scholar]
- Canut JA. Mandibular incisor extraction: indications and long-term evaluation. Eur J Orthod 1996; 18(5):485-9. doi: 10.1093/ejo/18.5.485 [Crossref] [ Google Scholar]
- Faerovig E, Zachrisson BU. Effects of mandibular incisor extraction on anterior occlusion in adults with class III malocclusion and reduced overbite. Am J Orthod Dentofacial Orthop 1999; 115(2):113-24. doi: 10.1016/s0889-5406(99)70337-9 [Crossref] [ Google Scholar]
- Hinkle F. Incisor extraction case report. Am J Orthod Dentofacial Orthop 1987; 92(2):94-7. doi: 10.1016/0889-5406(87)90363-5 [Crossref] [ Google Scholar]
- Brandt S, Safirstein GR. Different extractions for different malocclusions. Am J Orthod 1975; 68(1):15-41. doi: 10.1016/0002-9416(75)90157-8 [Crossref] [ Google Scholar]
- Dacre JT. The long term effects of one lower incisor extraction. Eur J Orthod 1985; 7(2):136-44. doi: 10.1093/ejo/7.2.136 [Crossref] [ Google Scholar]
- Sheridan JJ, Hastings J. Air-rotor stripping and lower incisor extraction treatment. J Clin Orthod 1992; 26(1):18-22. [ Google Scholar]
- Uribe F, Holliday B, Nanda R. Incidence of open gingival embrasures after mandibular incisor extractions: a clinical photographic evaluation. Am J Orthod Dentofacial Orthop 2011; 139(1):49-54. doi: 10.1016/j.ajodo.2009.03.049 [Crossref] [ Google Scholar]
- Biondi G. [Extraction of a lower incisor in adult orthodontic treatment: an acceptable compromise?]. Int Orthod 2006; 4(1):63-72. doi: 10.1016/s1761-7227(06)70221-2 [Crossref] [ Google Scholar]
- Miller RJ, Duong TT, Derakhshan M. Lower incisor extraction treatment with the Invisalign system. J Clin Orthod 2002; 36(2):95-102. [ Google Scholar]
- Valinoti JR. Mandibular incisor extraction therapy. Am J Orthod Dentofacial Orthop 1994; 105(2):107-16. doi: 10.1016/s0889-5406(94)70106-7 [Crossref] [ Google Scholar]
- Klein DJ. The mandibular central incisor, an extraction option. Am J Orthod Dentofacial Orthop 1997; 111(3):253-9. doi: 10.1016/s0889-5406(97)70182-3 [Crossref] [ Google Scholar]
- Riedel RA, Little RM, Bui TD. Mandibular incisor extraction--postretention evaluation of stability and relapse. Angle Orthod 1992; 62(2):103-16. doi: 10.1043/0003-3219(1992)062<0103:miepeo>2.0.co;2 [Crossref] [ Google Scholar]
- Hwang S, Kim I, Jang W, Choi YJ, Chung CJ, Kim KH. A 15-year follow up of an orthodontic treatment including a lower incisor extraction and keeping the maxillary canine-premolar transposition. Angle Orthod 2019; 89(5):812-26. doi: 10.2319/020118-93.1 [Crossref] [ Google Scholar]
- Berbert M, Cotrin P, de Oliveira RCG, de Oliveira RG, Valarelli FP, de Freitas MR. The influence of 3x3 bonded retainer on anterior crowding relapse in mandibular incisor extraction cases. Dental Press J Orthod 2021; 26(6):e212081. doi: 10.1590/2177-6709.26.6.e212081.oar [Crossref] [ Google Scholar]
- Vignesh T, Senthil Kumar KP, Tamizharasi SK. Mandibular incisor extraction in orthodontics: a systematic review. J Indian Acad Dent Spec Res 2014; 1(1):1-5. doi: 10.4103/2229-3019.135408 [Crossref] [ Google Scholar]
- Ajwa N, Albarkheel H, Alammar L, Alwoseamer A, Alhassoun A, Aljoudi J. The considerations of mandibular incisor extraction in orthodontic treatment: a systematic. Ann Dent Spec 2021; 9(2):42-51. doi: 10.51847/oFHM5pCzUw [Crossref] [ Google Scholar]
- Zhylich D, Suri S. Mandibular incisor extraction: a systematic review of an uncommon extraction choice in orthodontic treatment. J Orthod 2011; 38(3):185-95. doi: 10.1179/14653121141452 [Crossref] [ Google Scholar]
- de Almeida NV, Silveira GS, Pereira DM, Mattos CT, Mucha JN. Interproximal wear versus incisors extraction to solve anterior lower crowding: a systematic review. Dental Press J Orthod 2015; 20(1):66-73. doi: 10.1590/2176-9451.20.1.066-073.oar [Crossref] [ Google Scholar]
- Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2000. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Goldet G, Howick J. Understanding GRADE: an introduction. J Evid Based Med 2013; 6(1):50-4. doi: 10.1111/jebm.12018 [Crossref] [ Google Scholar]
- Mahmoudzadeh M, Mirzaei H, Farhadian M, Mollabashi V, Khosravi M. Comparison of anterior crowding relapse tendency in patients treated with incisor extraction, premolar extraction, and nonextraction treatment. J World Fed Orthod 2018; 7(2):61-5. doi: 10.1016/j.ejwf.2018.03.002 [Crossref] [ Google Scholar]
- Verma P, Jain RK. Comparative evaluation of stability of mandibular anterior crowding correction done with two different treatment protocols: a retrospective study. J Int Oral Health 2022; 14(2):189-94. doi: 10.4103/jioh.jioh_260_21 [Crossref] [ Google Scholar]
- Ileri Z, Basciftci FA, Malkoc S, Ramoglu SI. Comparison of the outcomes of the lower incisor extraction, premolar extraction and non-extraction treatments. Eur J Orthod 2012; 34(6):681-5. doi: 10.1093/ejo/cjr064 [Crossref] [ Google Scholar]
- Kamal AT, Shaikh A, Fida M. Improvement in Peer Assessment Rating scores after nonextraction, premolar extraction, and mandibular incisor extraction treatments in patients with class I malocclusion. Am J Orthod Dentofacial Orthop 2017; 151(4):685-90. doi: 10.1016/j.ajodo.2016.09.016 [Crossref] [ Google Scholar]
- Lee S, Firth FA, Bennani F, Harding W, Farella M, Antoun JS. Evaluation of objective and subjective treatment outcomes in orthodontic cases treated with extraction of a mandibular incisor. Angle Orthod 2019; 89(6):862-7. doi: 10.2319/011018-25.1 [Crossref] [ Google Scholar]
- Maaz M, Fida M. Comparison of treatment outcomes as assessed by 3 indexes in subjects with class I malocclusion treated by 3 different methods: a cross-sectional study. Am J Orthod Dentofacial Orthop 2022; 161(4):537-41. doi: 10.1016/j.ajodo.2020.10.031 [Crossref] [ Google Scholar]
- Barili F, Parolari A, Kappetein PA, Freemantle N. Statistical Primer: heterogeneity, random- or fixed-effects model analyses?. Interact Cardiovasc Thorac Surg 2018; 27(3):317-21. doi: 10.1093/icvts/ivy163 [Crossref] [ Google Scholar]
- Taner TU, Ciger S, El H, Germeç D, Es A. Evaluation of dental arch width and form changes after orthodontic treatment and retention with a new computerized method. Am J Orthod Dentofacial Orthop 2004; 126(4):464-75. doi: 10.1016/j.ajodo.2003.08.033 [Crossref] [ Google Scholar]
- Burke SP, Silveira AM, Goldsmith LJ, Yancey JM, Van Stewart A, Scarfe WC. A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod 1998; 68(1):53-60. doi: 10.1043/0003-3219(1998)068<0053:amaomi>2.3.co;2 [Crossref] [ Google Scholar]
- Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR Index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod 1992; 14(3):180-7. doi: 10.1093/ejo/14.3.180 [Crossref] [ Google Scholar]
- BeGole EA, Sadowsky C. Methodologies for evaluating long-term stability of dental relationships after orthodontic treatment. Semin Orthod 1999; 5(3):142-50. doi: 10.1016/s1073-8746(99)80005-x [Crossref] [ Google Scholar]
- Birkeland K, Furevik J, Bøe OE, Wisth PJ. Evaluation of treatment and post-treatment changes by the PAR Index. Eur J Orthod 1997; 19(3):279-88. doi: 10.1093/ejo/19.3.279 [Crossref] [ Google Scholar]