J Dent Res Dent Clin Dent Prospects. 18(3):189-195.
doi: 10.34172/joddd.41265
Original Article
Effect of thermomechanical aging on marginal fit of three CAD-CAM restorative materials: An in vitro study
Reda Eid Attia Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing, * 
Hussein Ramadan Mohammed Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Writing – review & editing, 
Khaled Mohamed Haggag Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Validation, Writing – review & editing, 
Author information:
Crown and Bridge Department, Faculty of Dental Medicine, Al Azhar University, Assiut, Egypt
Abstract
Background.
The present study assessed the impact of thermomechanical aging on the marginal fit of hybrid ceramic, reinforced composite resin, and lithium disilicate ceramic.
Methods.
Eighteen human upper first premolars freshly extracted for orthodontic purposes were used to fabricate 18 CAD-CAM veneers and divided into three groups based on materials used: group H (n=6): hybrid ceramics (Vita Enamic), group R (n=6): reinforced composite resin (Brilliant crios), and group L (n=6): lithium disilicate ceramic (IPS e-max CAD). Each material’s cementation procedure was carried out according to the manufacturer’s instructions. The vertical marginal gap between the laminate veneer margin and the prepared tooth finish line was measured to assess the specimens by digital microscopy. Subsequently, all the samples were thermomechanically cycled (TMC) (5 °C to 55 °C, 30 seconds, 75000 cycles). Then, the vertical marginal gap was re-evaluated.
Results.
The Brilliant crios group displayed a significantly lower vertical marginal gap mean score (31.36±2.82 µm) followed by Vita Enamic (39.27±6.54 µm) and E max (41.39±3.97 µm) groups. Similarly, after thermomechanical aging, the Brilliant crios group displayed a significantly lower vertical marginal gap mean score (41.83±8.28 µm) followed by Vita Enamic (55.47±18.65 µm), and the E max group showed the greatest vertical marginal gap mean score (59.43±16.27 µm).
Conclusion.
Thermomechanical aging affected the marginal fit of different materials employed in the current research, and these changes were under the established clinical limit.
Keywords: CAD/CAM, Hybrid ceramics, Marginal fit, Reinforced composite resin, Thermomechanical aging
Copyright and License Information
©2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
No funding.
Introduction
Laminate veneers are indirect restorations that restore adequate shape and function and harmonize the smile and color of aesthetically compromised teeth.1 The material of choice for laminate veneers is dental ceramic because of its esthetic advantages, including improved fluorescence, increased translucency,2 and high capacity to mimic tooth structure. In addition, dental ceramics are inert, biocompatible, and resistant to corrosion and have low electrical and temperature conductivity.3,4
In addition to the aesthetics and mechanical strength of any restoration,5 marginal fit is an essential requirement that must be carefully considered in the final restoration.6 Possible spaces might form across the prepared tooth and the external restoration boundary due to an inadequate fit. As these spaces increase, and as the majority of luting cement dissolves in oral fluids, bacterial plaque may accumulate in such compromised regions, causing pulpal lesions, caries, and gingival irritation. Additionally, disturbances in the fit can create stress concentrations and weaken the restoration, ultimately leading to its fracture.7
The globe’s initial hybrid dental ceramic with a double network design is called Vita Enamic. The acrylate polymer network in this dental material reinforces the predominate fine-structure ceramic network (86% by weight), and both networks are completely interwoven.8
Creating resin matrices for CAD-CAM blocks is a crucial step in optimizing CAD-CAM substances. Novel materials known as hybrids may be further classified into two categories depending on their chemical formulations: materials with a predominance of ceramic elements, known as resin nanoceramics, and materials primarily composed of resin matrix, known as nanohybrid composite resins. Brilliant crios (BC) is a novel CAD-CAM material that is a nanohybrid composite resin block. Backed by a strongly cross-linked methacrylate matrix, BC’s composition comprises around 71 wt% of inorganic filler that grasps 20-μm silica and 1-μm barium glass, leading to superior marginal performance over glass ceramics and increased dentin adhesion.9
Since BC’s modulus of elasticity is similar to that of dentin, which is significantly lower than that of ceramics, it creates a unique biomechanical compound (monoblock), where the restoration and tooth work together to more uniformly distribute force and increase the flexural strength.9 Furthermore, the reinforced composite has outstanding mechanical qualities thanks to controlled manufacturing and continuous heat curing, which might make them ideal for use in locations with strong occlusal stresses.10
Lithium disilicate ceramic is one of the ceramic systems used to fabricate monolithic restorations. Due to its better physical qualities and aesthetics, it has been successful over a long period. It is, therefore, more widely accepted for the restoration of the anterior and posterior teeth.11,12
There are variations as to the extent to which the marginal fit is considered clinically acceptable. McLean and von Fraunhofer13 proposed that in clinical terms, the restoration’s margin is deemed acceptable if the cement thickness and marginal gaps are < 120 µm.
Fransson et al14 showed that following cementation, a marginal gap of < 150 µm ought to be considered clinically acceptable. Another research proposed that it might be deemed acceptable whenever the marginal fit is invisible to the human eye or cannot be found using a dental probe.15,16 Moreover, Mclean and von Fraunhofer13 evaluated the marginal fit of 1000 fixed restorations for five years, concluding that it is challenging to identify a marginal gap measuring < 80 μm in a clinical setting.
There are four basic techniques for marginal fit measurement: direct view, cross-sectional view, impression replica method, and explorer and visual inspection.17
It is important to evaluate how different kinds of veneer materials behave in the oral cavity to fabricate durable veneers for patients. Variables in the oral cavity, including temperature, pH, humidity, and the veneer material’s resistance to such alterations, impact their durability over time.18,19 To assess the restorative materials’ capacity to remain unaltered, artificially accelerated aging is used to replicate the oral environmental circumstances.20
The current in vitro study assessed the impact of thermomechanical aging on the marginal fitof ceramic veneers made from VITA Enamic, Brilliant Crios, and IPS e-max CAD.
Methods
Table 1 lists the materials used in this study.Based on a previous study,18 upper first premolars recently extracted for orthodontic purposes were chosen.21 The premolars had no decay, microfractures, or abrasion cavitiesand did not have endodontic treatment in the past with a somewhat comparable size and form. The chosen premolars were divided equally into three groups according to the type of ceramic materials used to construct laminate veneers.
Table 1.
The materials used in this study
|
Materials
|
Composition
|
Manufacturer
|
LotNo
|
Dental hybrid ceramic
Vita Enamic |
-Ceramic part 86 %
(SiO2, Al2O3, Na2O, K2O, ZrO2)
-Polymer part 14 % (UDMA, TEGDMA) |
VITA
Zahnfabrik, Germany |
61960 |
Nano ceramic reinforced resin composite
Brilliant crios |
Barium glass < 1.0 µm, Amorphous silica SiO < 20 nm
Resin matrix: Cross-linked methacrylates
Pigments: ferrous oxide and titanium dioxide. |
Coltene/Whaledent AG, Switzerland |
L 33922 |
| Lithium Disilicate IPS e-max CAD |
SiO2
Additional contents (Al2O3, K2O, CaO, Na2O, other oxides) |
Ivoclar Vivadent AG, Schaan/ Liechtenstein Germany |
Z01SBK |
A custom-made Teflon mold was machine-milled and used to fabricate resin blocks. Each premolar was mounted separately using a self-cured acrylic resin (Acrostone Dental Factory, England.) vertically along its long axis. A hollow cylinder with an internal diameter of 2 cm and a depth of 2 cm was placed in the mold. The mold was held on the base of the paralleling device (Paraflex, Bego, Bremer, Germany) by screws. Each premolar was fixed to the lower tip of the device via a sticky wax; then, the tip was moved down to the predetermined depth, where the cervical line was 1 mm away from the self-cured acrylic resin, and waited for the final setting. The putty consistency of additional silicon impression material (Via L. Longo, 18-50019, Sesto F.no, Firenze, Italy) was used to create indexes for each tooth, ensuring uniform tooth preparation.
The natural tooth was prepared using a standardized preparation bur set (6926 Via al Molino 107, Switzerland) for ceramic laminate veneer fabrication. Occlusal reduction was approximately 1.5-mm22 clearance, and preparation went 2 mm toward the central groove. The buccal reduction was 0.5 mm. The proximal reduction was positioned immediately after the mediolabial and distolabial line angles. The cervical margin was positioned 1 mm23 occlusal to the cementoenamel junction. The preparation margin was surrounded by a chamfer finish line; its continuity and consistency were examined, and a rubber index was used to assess the degree of tooth reduction.
All restorations were fabricated by CAD-CAM system (Imes-Icore CAD-CAM System. Germany), which consists of a personal computer, a DOF scanner (Degree of Freedom Scanner, Korean), and an Imes-Icore milling unit. The in-lab user interface window was used to enter the restoration information. Veneer was chosen as the restoration type, and the upper first premolar was selected as the tooth and design mode. In the next step, the operator started the scanning process using Telescan spray (DFS-Diamon GmbH-Germany) to facilitate the acquisition of optical impressions for the prepared teeth. Scanning was carried out by a movable camera with a 3-axis scanning arm, which made it easier and quicker.
The laminate veneers were designed by the Exocad system (Exocad GmbH, Julius-Reiber-Str. 37, D-64293 Darmstadt), and restoration parameters were set, including spacer thickness (50 µm), the minimum thickness of the material. The model tooth veneer was selected, loaded, and placed on the virtual die image. The milling procedure was initiated by activating the milling preview window via a 5-axis dental milling machine. The milling procedure was accomplished with an abundant spray of water. Following the milling procedure, a low-speed diamond bur (Komit, Gebr, Brassrler, Lemgo, Germany) was used to eliminate excess material at the point of junction with the ceramic block and divide the fully milled restorations.
Based on the manufacturer’s directions, polishing, and finishing procedures were applied to Vita Enamic CAD/CAM restorations using a two-stage Vita Enamic polishing kit (Vita Zahnfabric, Bad Sackingen, Germany). The restorations made by Brilliant crios were subjected to finishing and polishing procedures using a Diatech finishing and polishing kit. (Coltene/Whaledent AG, Switzerland) The programat P310 oven (Ivoclar Vivadent AG Bendererstr. 29494 Schwan Liechtenstein, Germany) was used for the crystallization of IPS e.max CAD specimens and fired on their special firing tray based on the manufacturer’s instructions.
The inner surfaces of the Vita Enamic specimens were etched with 5% hydrofluoric acid (HF) for 60 seconds (Bisco, Inc. 1100 W, Schaumburg, IL 60193 U.S. A), rinsed, and air-dried based on the supplier recommendations and placed in an ultrasonic cleaner (Vita Sonic II, Germany) with distilled water for 5 minutes to remove the acid and debris remaining after acid etching. A silane coupling agent was applied for 60 seconds (Bisco, Inc. Schaumburg, USA) and left to dry.
The inner surfaces of the Brilliant crios specimens were sandblasted with 40-μm aluminum oxide particles at 1.5 bar for 15 seconds from a distance of 10 mm perpendicular to the inner surface of the specimen using the sandblasting device and bonded with a special bonding agent (One Coat 7 Universal) for Brilliant crios (Coltene Ltd – 60019539, Switzerland).
The inner surfaces of the E-max specimens were acid-etched with 9.5% HF for 20 seconds, followed by a 60-second water washing and placing in an ultrasonic cleaner for 5 minutes to remove the acid and debris remaining after acid etching. A silane coupling agent was applied to the inner surface for 60 seconds.
The enamel surface of all the teeth used in this study was etched with 37% phosphoric acid gel for 30 seconds (Madespa S.A Calle Río. Jarama, 12045007 Toledo), washed for 15 seconds with plenty of water, and air-dried. A universal adhesive (All Bond Universal Adhesive, Bisco, Inc.1100 Schaumburg, IL, 60193, USA) was applied to the etched enamel and allowed 15 seconds for reaction followed by 5 seconds of air drying without light curing according to manufacturer’s instructions.
The light-cured resin cement Choice 2 (Bisco, Inc., Schaumburg, USA) was applied to the produced veneer bonding surface. A specifically made cementing tool was used to provide a constant stress of 1 kg for 20 seconds24 on the buccal surface of the veneers that had been cemented.
The excess cement was light-cured for 2 seconds, eliminated with an explorer while the cement was still in its gel condition, and each veneer surface was light-cured again for 15 seconds at 1400 mW/cm2 (Monitex, LiteQ LD-107, Cordless LED Curing Light, Taiwan). Each tooth was again immersed in 37 ºC distilled water after restorative bonding until assessment.
Marginal fit evaluation before thermomechanical aging
The specimens (n = 6 in each group) were captured on video using a USB digital microscope with an integrated camera (U500X Digital Microscope, Guangdong, China) fixedly magnified by × 40 and linked to a suitable laptop.
The gap size was determined and assessed via a computerized image analysis program (Image J 1.43U, National Institute of Health, USA). All boundaries, dimensions, frames, and assessed parameters within the ImageJ program were given in pixels. Consequently, system calibration was carried out to translate the pixels into exact real-world units. A ruler (a recognized element utilized in the current study) was compared to a scale produced by the ImageJ program for calibration. The specimens were kept in position with a specially created holding mechanism.
For every specimen, shots of the margins were obtained. After that, morphometric measurements were made for every picture using three marks spaced equally throughout each surface’s perimeter. Every point was then measured three times. The acquired data were gathered, tabulated, and then subjected to statistical analyses.
Thermomechanical cyclic loading
For thermal cyclic aging, 7500 cycles were employed. Every water bath had a dwell time of 25 seconds and a lag time of 10 seconds. The minimum temperature level was 5ºC while the maximum temperature level was 55 ºC. A computerized logic-controlled apparatus was used for mechanical aging; a servomotor was used to run the recently created four-station multimodal ROBOTA chewing simulator combined via a thermocycling process. In the bottom sample holder, the samples were implanted in Teflon casing. Five kilograms of weight was used, corresponding to 49 N of chewing force. To simulate six months of chewing situation clinically, the examination was performed 75 000 times.
Marginal fit evaluation after thermomechanical aging
After the thermomechanical aging of specimens, the vertical marginal gap was measured using the same technique as before thermomechanical aging.
Statistical analysis
Means and standard deviations were used to describe the data, following confirmation of the normal distribution of errors and the uniformity of variance. Post hoc Tukey tests were used when the results of one-way ANOVA indicated statistical significance. The significance level was set at P ≤ 0.05.
Results
Vertical marginal gap (μm) results as mean and standard deviation (SD) values for all groups before and after thermomechanical aging are summarized in Table 2 and graphically drawn in Figure 1.
Table 2.
Vertical marginal gap results (Mean values ± SDs) for all the groups before and after thermomechanical aging
|
Variable
|
Thermomechanical aging
|
Statistics
|
|
Before
|
After
|
|
Mean
|
±SD
|
95% CI
|
Mean
|
±SD
|
95% CI
|
t-test
|
|
Low
|
High
|
Low
|
High
|
P
value
|
| Material group |
Vita Enamic |
39.27A |
6.54 |
35.57 |
42.97 |
55.47A |
18.65 |
63.3 |
70.32 |
< 0.0001* |
| Brilliant crios |
31.36B |
2.82 |
29.77 |
32.96 |
41.83B |
8.28 |
37.14 |
46.51 |
0.004* |
| E.max CAD |
41.39A |
3.97 |
39.15 |
43.64 |
59.43A |
16.27 |
51.92 |
84.4 |
0.0075* |
| Statistics |
ANOVA |
P value |
0.0003* |
P value |
0.0008* |
|
* Statistically significant.
Values with same superscript letter are not significantly different.
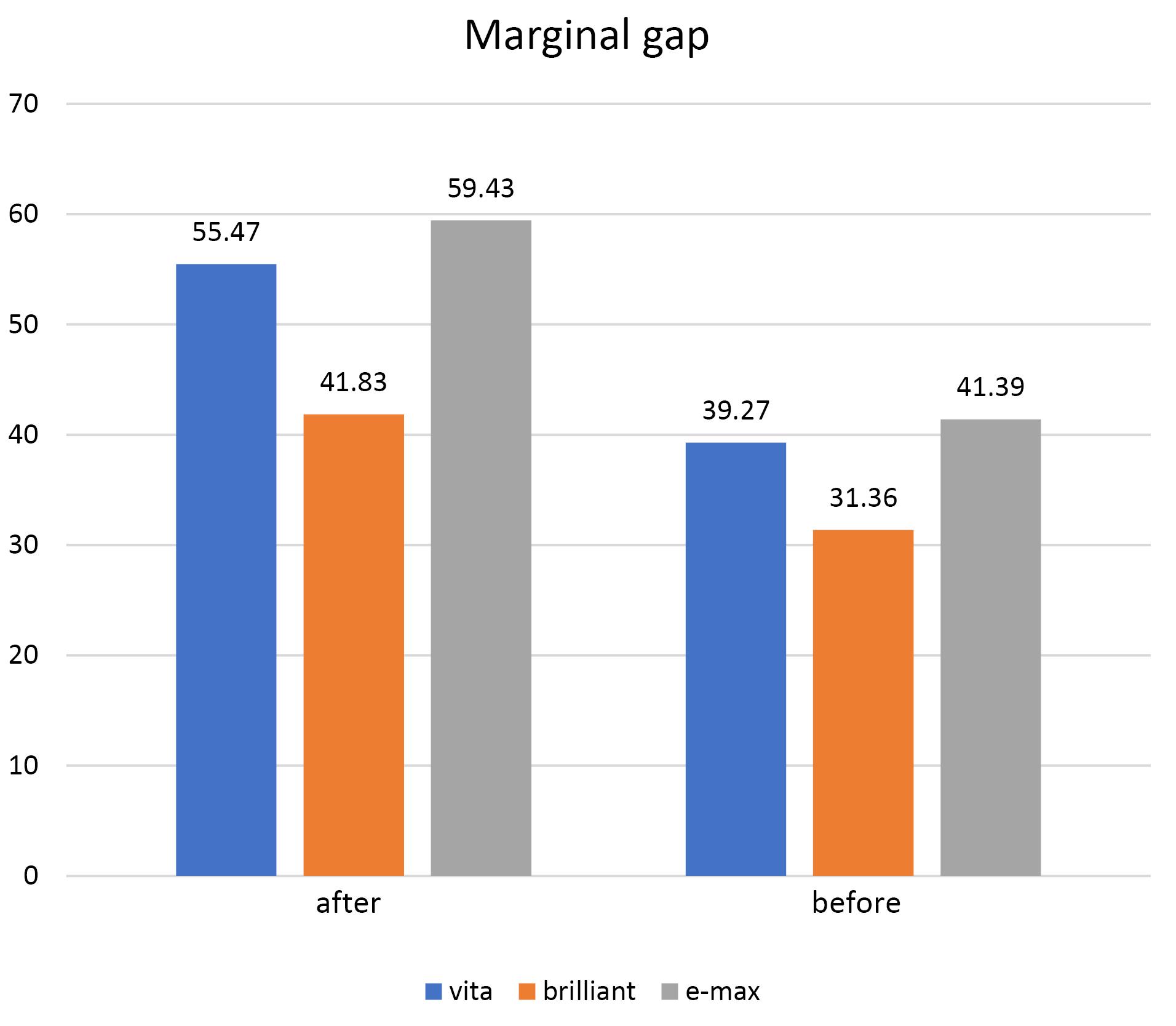
Figure 1.
Vertical marginal gap (μm) values for all groups before and after thermomechanical aging
.
Vertical marginal gap (μm) values for all groups before and after thermomechanical aging
Vita Enamic group recorded a significantly higher vertical marginal gap mean value after aging (55.47 μm) than before (39.27 μm) based on paired t-test (P ≤ 0.000). The Brilliant crios group exhibited significantly higher vertical marginal gap mean value after aging (41.83 ± 8.28 µm) than before aging (31.36 ± 2.82 µm) based on paired t-test (P = 0.0075). The e.max CAD group had a significantly higher vertical marginal gap mean value after aging (59.43 ± 16.27 µm) than before (41.39 ± 3.97 µm) based on paired t-test (P = 0.004).
Total effect of material group on marginal fit
Regardless of aging, the differences between groups were statistically significant according to two-way ANOVA (P = 0.0001) (e.max CAD ≥ Vita Enamic > Brilliant crios).
Aging’s impact on the marginal fit
Regardless of material groups, all the groups had a significantly higher mean value for the vertical marginal gap after aging than before, according to the two-way ANOVA (P ≤ 0.0001).
Table 2 and Figure 1 show vertical marginal gap results (mean ± SD) for all the groups before and after thermomechanical aging.
Discussion
Due to enhanced mechanical and optical properties, glass-matrix ceramics are frequently used for CAD/CAM restorations. Although they are well-established and successful materials, they have several disadvantages; due to hardness, glass-matrix ceramics have mechanical problems such as brittleness and abrasion on the opposing dentition.25
New restorative materials called polymer-infiltrated ceramics and composite CAD for use with CAD/CAM systems have been developed to improve the unfavorable properties of glass-matrix ceramics (high brittleness index and the need for further heat treatments after milling).26
The advantage of polymer-based materials is their good machinability, removing the need to fire restorations after milling. Also, they have a low brittleness index (which substantially reduces marginal chipping during the manufacturing process) and have elastic moduli comparable to those of natural tooth substances.27,28
Within the present research, every sample’s marginal fit was assessed at twelve different positions, three of which were at each of the four margins: the buccal, mesial, distal, and occlusal.29 The average value across all measurements was determined. Each evaluation was carried out by the same operator to minimize statistical variation.
The marginal fit was assessed using a digital microscope with a fixed magnification of × 40 for direct inspection and exterior evaluations.30 Because of its noninvasive nature, this measuring method helps determine the exact fit of the entire sample margin.
Extracted natural teeth were used as samples since they stimulate clinical situations more closely than resin abutments. For standardization purposes to decrease the differences between natural teeth and make the preparation more identical for all specimens, only maxillary first premolars with average dimensions were used in this study.31
Every single tooth was included in the silicone index before reduction for standardization. To prevent variations in preparation dimensions, standardized tooth preparation was carried out.32 For the optimal marginal fit, the recommended finish line types include shoulder-bevel, chamfer, and shoulder. Prior research revealed no distinction between the shoulder’s marginal fit and the chamfer margins; nonetheless, the chamfer design offers several clinical benefits over the shoulder design.33 For the best adhesion of the veneers to the tooth structure, the preparation must occur in the enamel; hence, 0.5–0.7 mm of enamel preparation is advised before applying veneers.34
The recently created four-station chewing simulator, powered by a servomotor and combined with a thermocycling protocol, carried out the cyclic loading procedure.35 A vertical load of 50 N was applied, which is thought to represent the mean of the physiological forces generated by mastication in non-bruxism patients’ teeth.36 A total of 75 000 cycles were completed, simulating six months of regular activity.35
Before thermomechanical aging, the Brilliant crios group showed a significantly lower vertical marginal gap average score (31.36 ± 2.82 µm) followed by Vita Enamic (39.27 ± 6.54 µm) and e-max group (41.39 ± 3.97 µm). Similarly, after thermomechanical aging, the Brilliant crios group showed a significantly lower vertical marginal gap average score (41.83 ± 8.28 µm), followed by Vita Enamic (55.47 ± 18.65 µm), and the e-max group showed the highest vertical marginal gap average score (59.43 ± 16.27 µm). These results rejected the null hypothesis.
Our research findings agreed with the investigation that assessed the marginal gaps between laminate veneers made using Lava Ultimate, IPS e-max CAD, and IPS Empress CAD on an epoxy resin die that had been produced and sealed using resin cement. All the samples’ marginal gaps were determined and documented before and after the artificially accelerated aging procedure. Both material type and aging process had a statistically significant impact on the marginal gap, which might be attributed to variations in the materials’ constitution. Restoration precision may be impacted by filler particle size and the kind of milling bur used. Additional factors include the CAD-CAM system’s inherent characteristics, the milling device’s rotary tool selection and speed, the production process, the preparation design, the spacer’s thickness, the precision of the scanning technique, the program system, and the kind of restorative material.37
Furthermore, compared to lithium disilicate ceramics, Brilliant crios materials are likely less brittle, contributing to this outcome. Because of its greater hardness, milling lithium disilicate requires more effort and time, which might raise the marginal disparity.38 Additionally, Azarbal et al39 have shown that the hardness of lithium disilicate may contribute to the wear of CAD/CAM milling burs because repetitive milling may impair the burs’ capability to cut, leading to increased marginal differences.
In the present study, thermomechanical aging caused a significant rise in the mean scores of the marginal gaps, which can be explained by the accelerated hydrolysis of unprotected collagen fibers and extraction of improper polymerized resin tags due to exposure to hot water. In addition, generated stresses at the tooth‒restoration interface because of a mismatch in the coefficient of thermal expansion of tooth structure and restorative material have been suggested as a crucial factor for deterioration of the marginal adaptability.40
These temperature alterations can cause expansion and contraction of the restorative materials, resulting in stresses, crack formation, and propagation due to an imbalance between the filler particles and the resin matrix’s coefficients of thermal expansion.41
Yao et al42 reported that the marginal accuracy of the CAD/CAM interim composite crowns did not change. Regarding the ideal marginal gap for ceramic crowns, a few studies have reported that the ideal marginal gap should be 25‒40 μm for cemented restorations.43 Other studies considered the marginal gap values of 100‒200 μm clinically acceptable for cemented restorations.44,45 More recent studies have evaluated the clinically good deals of the marginal gap to be less than 100 µm.30 Therefore, the results of marginal gaps for all groups presented in this study can be considered clinically acceptable.
One of the present study’s limitationswas thatthermomechanical aging was performed for a limited number of 7500 thermal cycles corresponding to only six months of clinical use, so more research is needed to simulate long-term oral performance for better evaluation of the durability of veneer restorations. Also, artificial saliva should be incorporated.
Conclusion
The subsequent clinical suggestion and conclusion might be made within the constraints of the present research:
-
Every restorative material that has been evaluated was susceptible to vertical marginal gap changes after being subjected to thermomechanical aging.
-
Brilliant crios material exhibited the least marginal gap before and after thermomechanical aging.
-
The vertical marginal gap of every material evaluated before and following thermomechanical loading was within the clinically acceptable limit.
Competing Interests
No competing interests.
Ethical Approval
This study was approved by the Research Ethics Committee Faculty of Dental Medicine, Al-Azhar University, under protocol number EC. Ref No:644/3634.
References
- Radz GM. Minimum thickness anterior porcelain restorations. Dent Clin North Am 2011; 55(2):353-70. doi: 10.1016/j.cden.2011.01.006 [Crossref] [ Google Scholar]
- Alqahtani MQ, Aljurais RM, Alshaafi MM. The effects of different shades of resin luting cement on the color of ceramic veneers. Dent Mater J 2012; 31(3):354-61. doi: 10.4012/dmj.2011-268 [Crossref] [ Google Scholar]
- Pecho OE, Ghinea R, Ionescu AM, de la Cruz Cardona J, Paravina RD, del Mar Pérez M. Color and translucency of zirconia ceramics, human dentine and bovine dentine. J Dent 2012; 40 Suppl 2:e34-40. doi: 10.1016/j.jdent.2012.08.018 [Crossref] [ Google Scholar]
- Wang F, Takahashi H, Iwasaki N. Translucency of dental ceramics with different thicknesses. J Prosthet Dent 2013; 110(1):14-20. doi: 10.1016/s0022-3913(13)60333-9 [Crossref] [ Google Scholar]
- Abdelhady WA, Metwally MF, Haggag KM. Effect of thermomechanical loading on fracture resistance and failure mode of new pressable zirconia-reinforced lithium disilicate onlay restoration. J Dent Res Dent Clin Dent Prospects 2024; 18(1):29-36. doi: 10.34172/joddd.40843 [Crossref] [ Google Scholar]
- Conrad HJ, Seong WJ, Pesun IJ. Current ceramic materials and systems with clinical recommendations: a systematic review. J Prosthet Dent 2007; 98(5):389-404. doi: 10.1016/s0022-3913(07)60124-3 [Crossref] [ Google Scholar]
- Balkaya MC, Cinar A, Pamuk S. Influence of firing cycles on the margin distortion of 3 all-ceramic crown systems. J Prosthet Dent 2005; 93(4):346-55. doi: 10.1016/j.prosdent.2005.02.003 [Crossref] [ Google Scholar]
- Bajraktarova-Valjakova E, Korunoska-Stevkovska V, Kapusevska B, Gigovski N, Bajraktarova-Misevska C, Grozdanov A. Contemporary dental ceramic materials, a review: chemical composition, physical and mechanical properties, indications for use. Open Access Maced J Med Sci 2018; 6(9):1742-55. doi: 10.3889/oamjms.2018.378 [Crossref] [ Google Scholar]
- Lin CL, Chang YH, Pai CA. Evaluation of failure risks in ceramic restorations for endodontically treated premolar with MOD preparation. Dent Mater 2011; 27(5):431-8. doi: 10.1016/j.dental.2010.10.026 [Crossref] [ Google Scholar]
- Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent 2015; 114(4):587-93. doi: 10.1016/j.prosdent.2015.04.016 [Crossref] [ Google Scholar]
- Bindl A, Richter B, Mörmann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. J Prosthet Dent 2006; 95(1):81. doi: 10.1016/j.prosdent.2005.09.002 [Crossref] [ Google Scholar]
- Guo J, Wang Z, Li X, Sun C, Gao E, Li H. A comparison of the fracture resistances of endodontically treated mandibular premolars restored with endocrowns and glass fiber post-core retained conventional crowns. J Adv Prosthodont 2016; 8(6):489-93. doi: 10.4047/jap.2016.8.6.489 [Crossref] [ Google Scholar]
- McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J 1971; 131(3):107-11. doi: 10.1038/sj.bdj.4802708 [Crossref] [ Google Scholar]
- Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater 1985; 1(5):197-9. doi: 10.1016/s0109-5641(85)80019-1 [Crossref] [ Google Scholar]
- Kokubo Y, Ohkubo C, Tsumita M, Miyashita A, Vult von Steyern P, Fukushima S. Clinical marginal and internal gaps of Procera AllCeram crowns. J Oral Rehabil 2005; 32(7):526-30. doi: 10.1111/j.1365-2842.2005.01458.x [Crossref] [ Google Scholar]
- Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int 2009; 40(3):243-50. [ Google Scholar]
- Sorensen JA. A standardized method for determination of crown margin fidelity. J Prosthet Dent 1990; 64(1):18-24. doi: 10.1016/0022-3913(90)90147-5 [Crossref] [ Google Scholar]
- Zarone F, Epifania E, Leone G, Sorrentino R, Ferrari M. Dynamometric assessment of the mechanical resistance of porcelain veneers related to tooth preparation: a comparison between two techniques. J Prosthet Dent 2006; 95(5):354-63. doi: 10.1016/j.prosdent.2006.03.003 [Crossref] [ Google Scholar]
- Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent 1996; 75(1):18-32. doi: 10.1016/s0022-3913(96)90413-8 [Crossref] [ Google Scholar]
- Turgut S, Bagis B. Colour stability of laminate veneers: an in vitro study. J Dent 2011; 39 Suppl 3:e57-64. doi: 10.1016/j.jdent.2011.11.006 [Crossref] [ Google Scholar]
- Silami FD, Tonani R, Alandia-Román CC, de Carvalho Panzeri Pires-de-Souza F. Influence of different types of resin luting agents on color stability of ceramic laminate veneers subjected to accelerated artificial aging. Braz Dent J 2016; 27(1):95-100. doi: 10.1590/0103-6440201600348 [Crossref] [ Google Scholar]
- Haralur SB. Microleakage of porcelain laminate veneers cemented with different bonding techniques. J Clin Exp Dent 2018; 10(2):e166-71. doi: 10.4317/jced.53954 [Crossref] [ Google Scholar]
- Akoğlu B, Gemalmaz D. Fracture resistance of ceramic veneers with different preparation designs. J Prosthodont 2011; 20(5):380-4. doi: 10.1111/j.1532-849X.2011.00728.x [Crossref] [ Google Scholar]
- Bompolaki D, Kontogiorgos E, Wilson JB, Nagy WW. Fracture resistance of lithium disilicate restorations after endodontic access preparation: an in vitro study. J Prosthet Dent 2015; 114(4):580-6. doi: 10.1016/j.prosdent.2015.04.013 [Crossref] [ Google Scholar]
- Stawarczyk B, Liebermann A, Eichberger M, Güth JF. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J Mech Behav Biomed Mater 2015; 55:1-11. doi: 10.1016/j.jmbbm.2015.10.004 [Crossref] [ Google Scholar]
- Lambert H, Durand JC, Jacquot B, Fages M. Dental biomaterials for chairside CAD/CAM: state of the art. J Adv Prosthodont 2017; 9(6):486-95. doi: 10.4047/jap.2017.9.6.486 [Crossref] [ Google Scholar]
- Alamoush RA, Kushnerev E, Yates JM, Satterthwaite JD, Silikas N. Response of two gingival cell lines to CAD/CAM composite blocks. Dent Mater 2020; 36(9):1214-25. doi: 10.1016/j.dental.2020.05.014 [Crossref] [ Google Scholar]
- Tsitrou EA, Northeast SE, van Noort R. Brittleness index of machinable dental materials and its relation to the marginal chipping factor. J Dent 2007; 35(12):897-902. doi: 10.1016/j.jdent.2007.07.002 [Crossref] [ Google Scholar]
- Sakrana AA. In vitro evaluation of the marginal and internal discrepancies of different esthetic restorations. J Appl Oral Sci 2013; 21(6):575-80. doi: 10.1590/1679-775720130064 [Crossref] [ Google Scholar]
- Holden JE, Goldstein GR, Hittelman EL, Clark EA. Comparison of the marginal fit of pressable ceramic to metal ceramic restorations. J Prosthodont 2009; 18(8):645-8. doi: 10.1111/j.1532-849X.2009.00497.x [Crossref] [ Google Scholar]
- Chitmongkolsuk S, Heydecke G, Stappert C, Strub JR. Fracture strength of all-ceramic lithium disilicate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur J Prosthodont Restor Dent 2002; 10(1):15-22. [ Google Scholar]
- Poiate IA, de Vasconcellos AB, de Santana RB, Poiate E. Three-dimensional stress distribution in the human periodontal ligament in masticatory, parafunctional, and trauma loads: finite element analysis. J Periodontol 2009; 80(11):1859-67. doi: 10.1902/jop.2009.090220 [Crossref] [ Google Scholar]
- Re D, Cerutti F, Augusti G, Cerutti A, Augusti D. Comparison of marginal fit of Lava CAD/CAM crown-copings with two finish lines. Int J Esthet Dent 2014; 9(3):426-35. [ Google Scholar]
- Chen XD, Hong G, Xing WZ, Wang YN. The influence of resin cements on the final color of ceramic veneers. J Prosthodont Res 2015; 59(3):172-7. doi: 10.1016/j.jpor.2015.03.001 [Crossref] [ Google Scholar]
- Nawafleh N, Hatamleh M, Elshiyab S, Mack F. Lithium disilicate restorations fatigue testing parameters: a systematic review. J Prosthodont 2016; 25(2):116-26. doi: 10.1111/jopr.12376 [Crossref] [ Google Scholar]
- Rupawala A, Musani SI, Madanshetty P, Dugal R, Shah UD, Sheth EJ. A study on the wear of enamel caused by monolithic zirconia and the subsequent phase transformation compared to two other ceramic systems. J Indian Prosthodont Soc 2017; 17(1):8-14. doi: 10.4103/0972-4052.194940 [Crossref] [ Google Scholar]
- Shim JS, Lee JS, Lee JY, Choi YJ, Shin SW, Ryu JJ. Effect of software version and parameter settings on the marginal and internal adaptation of crowns fabricated with the CAD/CAM system. J Appl Oral Sci 2015; 23(5):515-22. doi: 10.1590/1678-775720150081 [Crossref] [ Google Scholar]
- Yara A, Goto S, Ogura H. Correlation between accuracy of crowns fabricated using CAD/CAM and elastic deformation of CAD/CAM materials. Dent Mater J 2004; 23(4):572-6. doi: 10.4012/dmj.23.572 [Crossref] [ Google Scholar]
- Azarbal A, Azarbal M, Engelmeier RL, Kunkel TC. Marginal fit comparison of CAD/CAM crowns milled from two different materials. J Prosthodont 2018; 27(5):421-8. doi: 10.1111/jopr.12683 [Crossref] [ Google Scholar]
- Rosentritt M, Sikora M, Behr M, Handel G. In vitro fracture resistance and marginal adaptation of metallic and tooth-coloured post systems. J Oral Rehabil 2004; 31(7):675-81. doi: 10.1111/j.1365-2842.2004.01286.x [Crossref] [ Google Scholar]
- Morresi AL, D’Amario M, Monaco A, Rengo C, Grassi FR, Capogreco M. Effects of critical thermal cycling on the flexural strength of resin composites. J Oral Sci 2015; 57(2):137-43. doi: 10.2334/josnusd.57.137 [Crossref] [ Google Scholar]
- Yao J, Li J, Wang Y, Huang H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J Prosthet Dent 2014; 112(3):649-57. doi: 10.1016/j.prosdent.2014.01.012 [Crossref] [ Google Scholar]
- Hahnel S, Schultz S, Trempler C, Ach B, Handel G, Rosentritt M. Two-body wear of dental restorative materials. J Mech Behav Biomed Mater 2011; 4(3):237-44. doi: 10.1016/j.jmbbm.2010.06.001 [Crossref] [ Google Scholar]
- Baig MR, Tan KB, Nicholls JI. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J Prosthet Dent 2010; 104(4):216-27. doi: 10.1016/s0022-3913(10)60128-x [Crossref] [ Google Scholar]
- Pak HS, Han JS, Lee JB, Kim SH, Yang JH. Influence of porcelain veneering on the marginal fit of Digident and Lava CAD/CAM zirconia ceramic crowns. J Adv Prosthodont 2010; 2(2):33-8. doi: 10.4047/jap.2010.2.2.33 [Crossref] [ Google Scholar]