J Dent Res Dent Clin Dent Prospects. 18(3):204-209.
doi: 10.34172/joddd.41378
Original Article
Effect of different chelators on the push-out bond strength of hydraulic cements in retrograde obturation
Büşra Dağıstan-Çavuşoğlu Conceptualization, Data curation, Investigation, Methodology, 
Sıla Nur Usta Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing, * 
Author information:
Department of Endodontics, Gulhane Faculty of Dentistry, University of Health Sciences, Ankara, Turkey
Abstract
Background.
This study examined the effect of ethylenediaminetetraacetic acid (EDTA) and etidronic acid (HEDP) in retrograde cavities on the bond strength of MTA Angelus and NeoPutty.
Methods.
Sixty-six teeth with single roots and canals were decoronated and enlarged up to F3 using the ProTaper Universal file system. After removing the apical 3 mm within the scope of endodontic surgery procedures, retrograde cavities were prepared with ultrasonic tips. The teeth were divided into three main groups according to the irrigation solution used: saline, 17% EDTA, and 9% HEDP. Following the irrigation of retrograde cavities, each main group was further divided into two subgroups in terms of using MTA Angelus and NeoPutty as retrograde filling materials. Bond strength values of hydraulic cements were measured by the push-out test. Fracture modes were examined under a stereo microscope. Two dentin sections from each group were examined under scanning electron microscopy (SEM) to observe dentinal tubules. Two-way ANOVA and post hoc Tukey tests were used to analyze the data.
Results.
Irrigation solutions similarly affected the bond strength values of hydraulic cements (P=0.115). MTA Angelus showed significantly higher values than NeoPutty in all the solution groups (P=0.34). Adhesive and cohesive fracture modes were mostly observed in the MTA Angelus and NeoPutty groups, respectively.
Conclusion.
EDTA, HEDP, and saline had a similar effect on the bond strength of hydraulic cements. The higher bond values of MTA Angelus compared to NeoPutty could support its safe use in endodontic surgery procedures.
Keywords: EDTA, HEDP, MTA Angelus, NeoPutty, Push-out bond strength, Ultrasonic
Copyright and License Information
©2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The authors would like to thank Health Sciences University’s Scientific Research Committee for supporting this study (grant no: 2023/025).
Introduction
The success of root canal treatment depends on treating and/or preventing the formation of apical periodontitis by chemomechanical debridement of the root canal system to remove bacteria and their products.1 Although the success rate of root canal treatments in less than five years has been reported to be high, factors such as unretrievable broken files, persistent periradicular infections, and calcified root canals may jeopardize complete disinfection.2 Accordingly, endodontic root-end surgery can be performed due to its successful outcomes in such circumstances.3
Root-end surgery encompasses a hermetic retrograde obturation of the root-end cavity following a minimum 2-mm resection of the apical third to minimize bacterial leakage from the canals.4 In this sense, placing an ideally biocompatible root-end filling material with enhanced sealing ability is essential for successful outcomes.5 In particular, hydraulic cements are preferred due to their superior benefits for retrograde obturation. One of these materials, MTA Angelus (Angelus Indústria de Produtos Odontológicos S/A, Londrina, PR, Brazil), is generally used as the material of choice for root-end filling since it has most of the properties of an outstanding obturation material.6 In the literature, compatible results of MTA Angelus have been demonstrated in terms of bond strength and sealing ability.7,8 However, some drawbacks regarding the standardization of mixing and handling encourage the production of new materials.9 In recent years, NeoPutty (NuSmile, Houston, TX, USA) has been introduced to the dental markets as a premixed format of hydraulic cements that contains tantalum oxide, tricalcium silicate, calcium aluminate, dicalcium silicate, tricalcium aluminate, and calcium sulfate.10 According to the manufacturers, NeoPutty has lower solubility, dimensional expansion and adequate radiopacity.11 Additionally, the bioactive and biocompatible properties of NeoPutty allow it to be used in multi-purpose root and pulp treatments.12,13 In this sense, the compatible features of NeoPutty compared to MTA led to its use in root-end surgery procedures.10,12,14
A proper physical and biological structure must be provided to achieve good bonding between the root-end cavity and filling material. In particular, smear layer formation can alter the bond strength of root-end filling materials to dentin during root-end surgery applications. Ethylenediaminetetraacetic acid (EDTA) is frequently used to remove the inorganic components of the smear layer in routine endodontic practices.15 However, alternative chelating agents are being investigated since EDTA has low biocompatibility, is insufficient to remove the smear layer in the apical region of the root, and reduces the effectiveness of sodium hypochlorite (NaOCl) when used in combination.16,17 In this context, etidronic acid (1-hydroxyethylidene-1,1-bisphosphonate or HEDP) is increasingly regarded as a reliable chelating agent due to its adequate calcium chelation capacity and biocompatible structure. Unlike other chelators such as EDTA or citric acid, HEDP does not affect the antimicrobial/antibiofilm and tissue-dissolving properties of NaOCl when used in combination.18,19 Additionally, the more controlled demineralization effect of HEDP compared to EDTA helps preserve the sound dentin structure under the smear layer.20 In addition to its chelating features, it also has superior proteolytic and antimicrobial activity.21
Successful outcomes after root-end surgery applications entail high precision, experience, and suitable materials and techniques. In particular, minimizing the apical leakage with an advanced bonding between the root-end cavity dentin and the filling material is crucial. To our knowledge, the use of NeoPutty as a root-end filling material in contact with EDTA and HEDP has not been investigated yet. Thus, this in vitro study aimed to evaluate the effects of EDTA and HEDP on the bond strength of MTA Angelus and NeoPutty to root-end cavity dentin in endodontic surgery applications. The first null hypothesis of the study is that different solutions used in the root-end cavity would not differ in terms of affecting the bond strength values of hydraulic cements. The second null hypothesis of the study is that different hydraulic cements used in the root-end cavity would present similar bond strength values to dentin.
Methods
Sample size calculation and tooth selection
The protocol was approved by the Ethics Committee of the University (No.: 2023/12). The sample size was calculated based on a similar study in the literature22 with an effect size of 0.6641, type I error probability of 0.05, and a study power of 90%. Consequently, the total required number of teeth was determined at n = 60. In addition, for the scanning electron microscopy (SEM) analysis (Philips, FEI-Quanta 400 F, Netherlands), six teeth (two teeth per group) were also included. Sixty-six extracted human teeth with caries-free, single-rooted, mature apex and less than 10º curvature23 were collected and evaluated under a stereomicroscope for possible fractures or anatomical malformations. The exclusion criteria for the selected teeth were calcified root canals, external or internal root resorption, and apical constriction > #15 K-file (Dentsply Maillefer, Ballaigues, Switzerland). Subsequently, the periodontal tissues of the selected teeth were removed from the external root surfaces with periodontal curettes, and the teeth were stored in 0.1% thymol solution at 4 ºC until used.
Root canal preparation and obturation and application of root-end surgery protocols
The teeth were decoronated, and the root lengths were adjusted to 16 ± 1 mm. The working length was determined at 1 mm short of where a #15 K-file became visible at the apical foramen. The root canals were instrumented with ProTaper Universal (Dentsply Tulsa Dental, Tulsa, OK, USA) rotary file system up to F3. Between files, the root canals were irrigated with 2 mL of 5.25%5 NaOCl (Microvem, Istanbul, Turkey). Final irrigation was performed using 5.25% NaOCl, 17% EDTA (Imicryl Ltd., Konya, Turkey), and distilled water, respectively. Afterward, root canal systems were obturated using F3 gutta-percha (Bio GP Points, Gyeonggi-do, South Korea) and AH Plus sealer (Dentsply, DeTrey Gmbh, Konstanz, Germany) with lateral condensation technique.
Following root canal obturation, the apical 3 mm of the roots was resected under water cooling at a right angle to the long axis of the root to mimic endodontic surgical procedures. Root-end preparations were carried out using ultrasonic tips (E10D, Woodpecker Co., LTD, Guangxi, China). Then, the teeth were divided into three main groups randomly (https://www.randomizer.org/) in terms of the chelating agents as follows: 17% EDTA (n = 20, Imicryl Ltd., Konya, Turkey), 9% HEDP (n = 20, Dual Rinse, Medcem, Weinfelden, Switzerland), and 0.9% saline (n = 20). Root-end cavities were rinsed with 5 mL of each solution for 5 minutes.22
Three main groups were then divided into two subgroups in terms of root-end filling material as follows: MTA Angelus (n = 10, Angelus Indústria de Produtos Odontológicos S/A, Londrina, PR, Brazil) and NeoPutty (n = 10, NuSmile, Houston, TX, USA). Hydraulic cements were prepared and placed into root-end cavities according to the manufacturer’s instructions. The samples were incubated under 95% relative humidity at 37 °C for one week to mimic the clinical environment.
Effect of chelators on the bond strength of hydraulic cements and analysis of failure modes
One week later, the teeth were embedded in acrylic molds. Two slices of each tooth with ~1 mm thickness were obtained from the apicocoronal direction (IsoMet 1000, Buehler, IL, USA). Slices were placed in a universal testing machine (Lloyd LRX, Lloyd Instruments Ltd., Fareham, UK). A continuous load was applied to the center of the tested cement using a stainless-steel cylindrical plunger, measuring 0.7 mm24 in diameter, mounted on the machine. The push-out force was applied with a 1 mm/min crosshead speed in the coronoapical direction until bond failure occurred between the root dentin and the cement. The bond strength value was recorded in Newton (N) and calculated by converting these forces to Megapascals (MPa).
The fractured surfaces were examined under × 12 magnification under a stereomicroscope (Leica M165C, Leica Mycrosystems Ltd, Wetzlar, Germany). The failure modes were classified as adhesive, cohesive, and mixed.
SEM and statistical analysis
Six teeth (two from each solution group) were examined with SEM to observe the dentinal tubules (B.D.Ç.). In this context, dentin discs were vacuum-dried and coated with gold under 20 kV current; then, the samples were examined under × 5000 magnification, and images were taken. SEM images were evaluated by another researcher (S.N.U.) who was blinded to the groups.
Data were analyzed using SPSS 26 (Chicago, IL, USA). The Kolmogorov-Smirnov and Levene tests were used to check the normal distribution and homogeneity of data, respectively. Two-way ANOVA and post hoc Tukey tests were used to evaluate the effect of different irrigation solutions on the bond strength of MTA Angelus and NeoPutty. The level of significance was set at P < 0.05.
Results
SEM analysis revealed that while dentinal tubules were covered with the smear layer in the saline group, EDTA and HEDP were associated with smear layer removal efficiency (Figure 1).
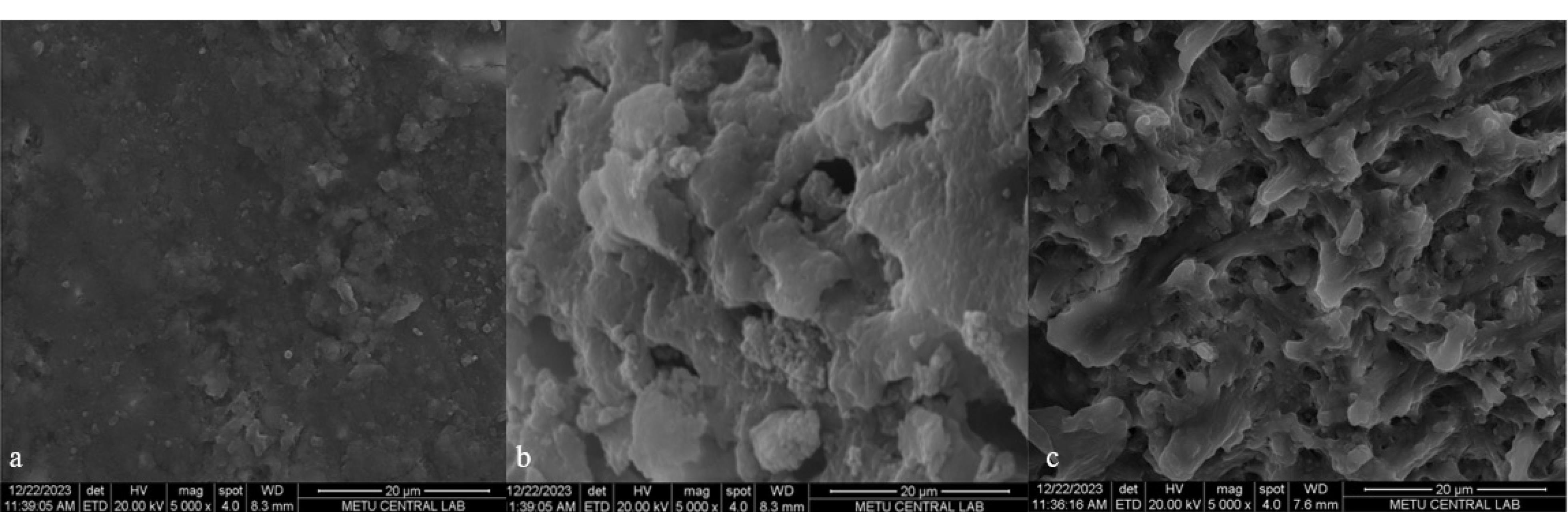
Figure 1.
SEM images of solution groups (a) saline, (b) EDTA, (c) HEDP
.
SEM images of solution groups (a) saline, (b) EDTA, (c) HEDP
Regardless of the root-end filling material, although higher bond strength values were observed in the saline group, no statistically significant difference was found between EDTA, HEDP, and saline groups (P = 0.115). The push-out bond strength values of MTA Angelus were significantly higher than NeoPutty in all irrigation solution groups (P = 0.34). Table 1 shows the main and standard deviations of bond strength values based on groups.
Table 1.
Mean ± standard deviation (SD) of the push-out bond strength values of the groups in terms of solutions and hydraulic cements
|
|
n
|
MTA Angelus
|
NeoPutty
|
Comparison
P
value
|
| Saline |
20 |
25.06 ± 9.15a,1 |
21.71 ± 4.80b,1 |
0.115 |
| EDTA |
20 |
20.54 ± 11.63a,1 |
15,50 ± 5.08b,1 |
| HEDP |
20 |
24.99 ± 10.64a,1 |
19.29 ± 6.18b,1 |
| Comparison P value |
|
0.034 |
|
Different superscript lowercase letters in the same row indicate a statistically significant difference (P < 0.05).
The same superscript numbers in the same column indicate no statistically significant difference (P > 0.05).
Figure 2 shows the failure modes.Cohesive, mixed, and adhesive failure modes were observed more frequently in the EDTA, HEDP, and saline groups, respectively. Moreover, adhesive and mixed failure modes were most common in the MTA Angelus group, while cohesive and mixed fracture modes were observed in the NeoPutty group. Table 2 presents the number and percentage of failure modes in each group.
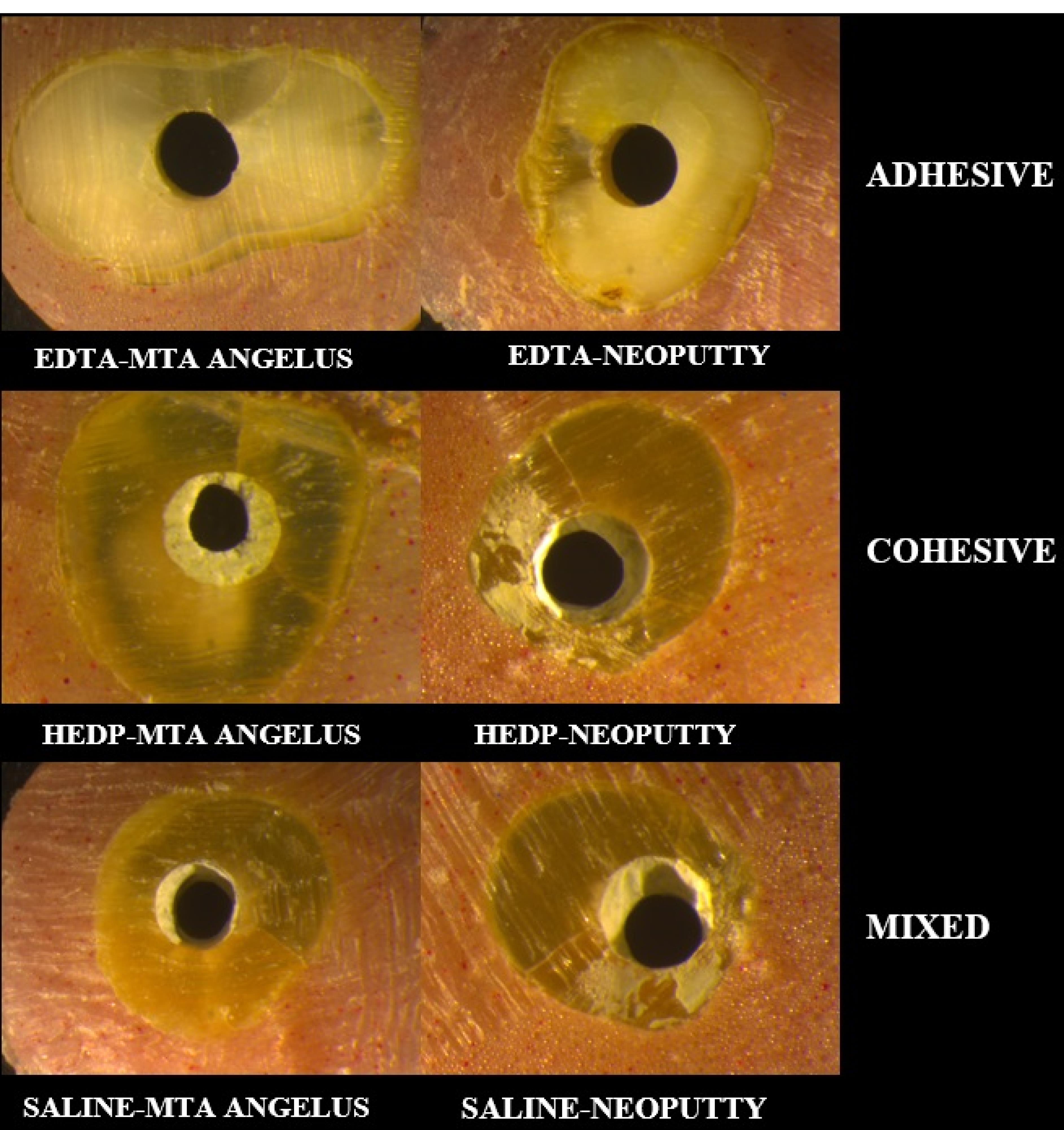
Figure 2.
Representative images of failure modes based on groups
.
Representative images of failure modes based on groups
Table 2.
Number and percentage of failure types for each group
|
Groups
|
N
|
Failure types (n (%))
|
|
Adhesive
|
Cohesive
|
Mixed
|
| EDTA-MTA Angelus |
20 |
6 (30%) |
6 (30%) |
8 (40%) |
| HEDP-MTA Angelus |
20 |
12 (60%) |
2 (10%) |
6 (30%) |
| Saline-MTA Angelus |
20 |
4 (20%) |
10 (50%) |
6 (30%) |
| EDTA-NeoPutty |
20 |
4 (20%) |
8 (40%) |
8 (40%) |
| HEDP-NeoPutty |
20 |
6 (30%) |
8 (40%) |
6 (30%) |
| Saline-NeoPutty |
20 |
6 (30%) |
8 (40%) |
6 (30%) |
Discussion
Clinical studies can demonstrate the outcomes of root-end surgery procedures effectively.25 However, well-designed in vitro studies are also needed to assess the possible effects of newly developed materials recommended for use in root-end cavities. In this sense, using NeoPutty as a relatively new material has not been investigated in root-end surgery applications. Moreover, possible interactions between NeoPutty and chelators in the apical thirds of teeth have not also been indicated. Therefore, this study aimed to signify the bond strength of NeoPutty in retrograde obturation in contact with EDTA and HEDP, compared with MTA Angelus. While the first null hypothesis was accepted, the second one was rejected since MTA Angelus and NeoPutty showed statistically significant differences.
A strong bond between retrograde obturation material and dentin is important to enhance the sealing ability and resist dislodgement forces.26 The filling material used and the physicochemical environment of the root-end cavity space resulting from solutions and blood contamination can be considered influential factors for adhesion.22,27 Accordingly, the chemical structure and setting properties of hydraulic cements may be affected by chelators. In this sense, conflicting results have been reported in the literature regarding the smear layer removal for a strong bond of hydraulic cements to the dentin.22,28 Since study designs and materials used have unique properties, diversities in the results prevent reaching a definite conclusion.
In this study, solutions did not differ in terms of affecting the bond strength of MTA Angelus and NeoPutty in root-end cavities, as in previous studies.22,29 However, the values were relatively higher and lower in saline and EDTA groups, respectively, which can be explained by the fact that EDTA was shown to hinder the hydration mechanism by chelating calcium ions released from hydraulic cements and reducing their chemical adhesion to dentin.30 Another reason for reduced values in the EDTA group could be the impaired surface hardness of hydraulic cements in an acidic environment.31 Valencia et al32 reported the improved bond strength of Portland cement when EDTA was used for smear layer removal. They attributed this result to the decreased contact surface at the material‒dentin interface and the intratubular formation of tail-like structures. The different results may be interpreted by the differences in exposure times and amounts of exposure to the solution, concentrations, material properties, and the investigated tooth part.
This study indicated similar values between HEDP and saline groups with no detrimental effects. One possible explanation could be the enhanced hydration of hydraulic cements that have been demonstrated by Neelakantan et al33 through the formation of a highly crystalline surface and a high release of calcium in samples of hydraulic cements after being wrapped in a gauze soaked in a mixture of 6% NaOCl and 18% HEBP. Moreover, Rebolloso de Barrio et al showed higher bond strength values of MTA after one day of exposure to NaOCl + HEDP.34 Ulusoy et al35 also reported higher dislodgement resistance of MTA in the HEDP group compared to EDTA. However, direct comparisons cannot be made since there is no information regarding the effect of HEDP on the adhesion of the MTA Angelus and NeoPutty in root-end cavities.
Although NeoPutty is suggested as a root-end filling material,10 the bond strength values were significantly lower compared to MTA Angelus, which can be explained by the different diffusion capacities of these cements into dentinal tubules. Another possible reason could be the particle size difference between MTA Angelus and NeoPutty. In this context, it was considered that MTA Angelus may contain larger particles due to the presence of bismuth oxide. Accordingly, larger particle sizes could help sustain higher loads.36 However, interestingly, MTA Angelus groups mainly exhibited adhesive and mixed types of failures. Although the large particle size of the material provides good adhesion in the superficial dentin, it is thought that it may have caused massive displacement as it prevented deep invasion into the dentinal tubules. In addition, it should also be remembered that the analysis of failure modes is not the sole criterion for assessing the bond strength.37
Although the push-out test is widely accepted and used to assess the bond strength of dentin to different materials, this method deserves attention,38 especially concerning the diameter of the plunger tips and samples used, the properties of the materials, and the applied force that might lead to different results across studies. In this sense, test set-up and sample sizes were determined according to the study performed by Chen et al24 to minimize the limitations. Moreover, using single-rooted tooth apical root sections allowed a highly standardized and reproducible protocol with samples of a constant thickness.28 Finally, since bond strength values can be interpreted within the scope of smear layer removal, observing dentinal tubules with SEM has implied a more accurate and effective evaluation process.
Conclusion
Comparable effects of HEDP with EDTA and saline support its use as a root-end filling material. NeoPutty showed lower push-out bond strength values than MTA Angelus. Future well-designed studies are needed to better evaluate the interaction between NeoPutty and dentin along with irrigation solutions.
Acknowledgments
The authors would like to thank Health Sciences University’s Scientific Research Committee for supporting this study (grant no: 2023/025).
Competing Interests
None.
Ethical Approval
The protocol of this study was approved by the Ethics Committee of the University of Health Sciences (Code: 2023/12).
References
- Huumonen S, Lenander-Lumikari M, Sigurdsson A, Ørstavik D. Healing of apical periodontitis after endodontic treatment: a comparison between a silicone-based and a zinc oxide-eugenol-based sealer. Int Endod J 2003; 36(4):296-301. doi: 10.1046/j.1365-2591.2003.00651.x [Crossref] [ Google Scholar]
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 2009; 35(7):930-7. doi: 10.1016/j.joen.2009.04.023 [Crossref] [ Google Scholar]
- Setzer FC, Kratchman SI. Present status and future directions: surgical endodontics. Int Endod J 2022; 55 Suppl 4:1020-58. doi: 10.1111/iej.13783 [Crossref] [ Google Scholar]
- Gilheany PA, Figdor D, Tyas MJ. Apical dentin permeability and microleakage associated with root end resection and retrograde filling. J Endod 1994; 20(1):22-6. doi: 10.1016/s0099-2399(06)80022-1 [Crossref] [ Google Scholar]
- Li H, Guo Z, Li C, Ma X, Wang Y, Zhou X. Materials for retrograde filling in root canal therapy. Cochrane Database Syst Rev 2021; 10(10):CD005517. doi: 10.1002/14651858.CD005517.pub3 [Crossref] [ Google Scholar]
- Falkowska J, Chady T, Dura W, Droździk A, Tomasik M, Marek E. The washout resistance of bioactive root-end filling materials. Materials (Basel) 2023; 16(17):5727. doi: 10.3390/ma16175757 [Crossref] [ Google Scholar]
- Xavier CB, Weismann R, de Oliveira MG, Demarco FF, Pozza DH. Root-end filling materials: apical microleakage and marginal adaptation. J Endod 2005; 31(7):539-42. doi: 10.1097/01.don.0000152297.10249.5a [Crossref] [ Google Scholar]
- Stefaneli Marques JH, Silva-Sousa YT, Rached-Júnior FJ, de Macedo LM, Mazzi-Chaves JF, Camilleri J. Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz Oral Res 2018; 32:e18. doi: 10.1590/1807-3107bor-2018.vol32.0018 [Crossref] [ Google Scholar]
- Camilleri J, Atmeh A, Li X, Meschi N. Present status and future directions: hydraulic materials for endodontic use. Int Endod J 2022; 55(Suppl 3):710-77. doi: 10.1111/iej.13709 [Crossref] [ Google Scholar]
- Rojas-Gutiérrez WJ, Pineda-Vélez E, Agudelo-Suárez AA. Regenerative endodontics success factors and their overall effectiveness: an umbrella review. Iran Endod J 2022; 17(3):90-105. doi: 10.22037/iej.v17i3.32703 [Crossref] [ Google Scholar]
- NeoPutty (NuSmile, Houston, TX, USA) brochure. [cited 13.01.2024]; Available from: https://cdn.shopify.com/s/files/1/0605/6729/0045/files/NeoPUTTY-Product-Sheet.pdf?v=1663792814.
- Lozano-Guillén A, López-García S, Rodríguez-Lozano FJ, Sanz JL, Lozano A, Llena C. Comparative cytocompatibility of the new calcium silicate-based cement NeoPUTTY versus NeoMTA Plus and MTA on human dental pulp cells: an in vitro study. Clin Oral Investig 2022; 26(12):7219-28. doi: 10.1007/s00784-022-04682-9 [Crossref] [ Google Scholar]
- Saber SM, Gomaa SM, Elashiry MM, El-Banna A, Schäfer E. Comparative biological properties of resin-free and resin-based calcium silicate-based endodontic repair materials on human periodontal ligament stem cells. Clin Oral Investig 2023; 27(11):6757-68. doi: 10.1007/s00784-023-05288-5 [Crossref] [ Google Scholar]
- Alqahtani AS, Alsuhaibani NN, Sulimany AM, Bawazir OA. NeoPUTTY® versus NeoMTA 2® as a pulpotomy medicament for primary molars: a randomized clinical trial. Pediatr Dent 2023; 45(3):240-4. [ Google Scholar]
- Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J 2014; 216(6):299-303. doi: 10.1038/sj.bdj.2014.204 [Crossref] [ Google Scholar]
- Zaccaro Scelza MF, da Silva Pierro VS, Chagas MA, da Silva LE, Scelza P. Evaluation of inflammatory response of EDTA, EDTA-T, and citric acid in animal model. J Endod 2010; 36(3):515-9. doi: 10.1016/j.joen.2009.11.011 [Crossref] [ Google Scholar]
- Zehnder M, Schmidlin P, Sener B, Waltimo T. Chelation in root canal therapy reconsidered. J Endod 2005; 31(11):817-20. doi: 10.1097/01.don.0000158233.59316.fe [Crossref] [ Google Scholar]
- Rath PP, Yiu CKY, Matinlinna JP, Kishen A, Neelakantan P. The effects of sequential and continuous chelation on dentin. Dent Mater 2020; 36(12):1655-65. doi: 10.1016/j.dental.2020.10.010 [Crossref] [ Google Scholar]
- Morago A, Ordinola-Zapata R, Ferrer-Luque CM, Baca P, Ruiz-Linares M, Arias-Moliz MT. Influence of smear layer on the antimicrobial activity of a sodium hypochlorite/etidronic acid irrigating solution in infected dentin. J Endod 2016; 42(11):1647-50. doi: 10.1016/j.joen.2016.07.023 [Crossref] [ Google Scholar]
- De-Deus G, Zehnder M, Reis C, Fidel S, Fidel RA, Galan J Jr. Longitudinal co-site optical microscopy study on the chelating ability of etidronate and EDTA using a comparative single-tooth model. J Endod 2008; 34(1):71-5. doi: 10.1016/j.joen.2007.09.020 [Crossref] [ Google Scholar]
- Álvarez-Sagües A, Herce N, Amador U, Llinares-Pinel F, Nistal-Villan E, Presa J. Efficacy of EDTA and HEDP chelators in the removal of mature biofilm of Enterococcus faecalis by PUI and XPF file activation. Dent J (Basel) 2021; 9(4):41. doi: 10.3390/dj9040041 [Crossref] [ Google Scholar]
- Ballal NV, Ulusoy Ö, Chhaparwal S, Ginjupalli K. Effect of novel chelating agents on the push-out bond strength of calcium silicate cements to the simulated root-end cavities. Microsc Res Tech 2018; 81(2):214-9. doi: 10.1002/jemt.22969 [Crossref] [ Google Scholar]
- Schilder H. Cleaning and shaping the root canal. Dent Clin North Am 1974; 18(2):269-96. [ Google Scholar]
- Chen WP, Chen YY, Huang SH, Lin CP. Limitations of push-out test in bond strength measurement. J Endod 2013; 39(2):283-7. doi: 10.1016/j.joen.2012.11.002 [Crossref] [ Google Scholar]
- Meschi N, Fieuws S, Vanhoenacker A, Strijbos O, Van der Veken D, Politis C. Root-end surgery with leucocyte- and platelet-rich fibrin and an occlusive membrane: a randomized controlled clinical trial on patients’ quality of life. Clin Oral Investig 2018; 22(6):2401-11. doi: 10.1007/s00784-018-2343-z [Crossref] [ Google Scholar]
- Mason J, Kirkpatrick T, Roberts HW. Dislodgement pushout resistance of five bioceramic root-end filling materials. Dent Mater J 2022; 41(6):843-9. doi: 10.4012/dmj.2022-058 [Crossref] [ Google Scholar]
- Gandolfi MG, Taddei P, Siboni F, Modena E, Ciapetti G, Prati C. Development of the foremost light-curable calcium-silicate MTA cement as root-end in oral surgery Chemical-physical properties, bioactivity and biological behavior. Dent Mater 2011; 27(7):e134-57. doi: 10.1016/j.dental.2011.03.011 [Crossref] [ Google Scholar]
- Rebolloso de Barrio E, Gancedo-Caravia L, García-Barbero E, Pérez-Higueras JJ. Effect of exposure to root canal irrigants on the push-out bond strength of calcium silicate-based cements. Clin Oral Investig 2021; 25(5):3267-74. doi: 10.1007/s00784-020-03658-x [Crossref] [ Google Scholar]
- Çelik D, Er K, Serper A, Taşdemir T, Ceyhanlı KT. Push-out bond strength of three calcium silicate cements to root canal dentine after two different irrigation regimes. Clin Oral Investig 2014; 18(4):1141-6. doi: 10.1007/s00784-013-1082-4 [Crossref] [ Google Scholar]
- Lee YL, Lin FH, Wang WH, Ritchie HH, Lan WH, Lin CP. Effects of EDTA on the hydration mechanism of mineral trioxide aggregate. J Dent Res 2007; 86(6):534-8. doi: 10.1177/154405910708600609 [Crossref] [ Google Scholar]
- Namazikhah MS, Nekoofar MH, Sheykhrezae MS, Salariyeh S, Hayes SJ, Bryant ST. The effect of pH on surface hardness and microstructure of mineral trioxide aggregate. Int Endod J 2008; 41(2):108-16. doi: 10.1111/j.1365-2591.2007.01325.x [Crossref] [ Google Scholar]
- Valencia YM, Vertuan GC, Alcalde MP, Vivan RR, Reis Só MV, Duarte MAH. Effect of irrigating agitation after root end preparation on the wall cleaning and bond strength of calcium silicate material in retrograde obturation. Eur J Dent 2021; 15(4):707-13. doi: 10.1055/s-0041-1729454 [Crossref] [ Google Scholar]
- Neelakantan P, Berger T, Primus C, Shemesh H, Wesselink PR. Acidic and alkaline chemicals’ influence on a tricalcium silicate-based dental biomaterial. J Biomed Mater Res B Appl Biomater 2019; 107(2):377-87. doi: 10.1002/jbm.b.34129 [Crossref] [ Google Scholar]
- Rebolloso de Barrio E, Pérez-Higueras JJ, García-Barbero E, Gancedo-Caravia L. Effect of exposure to etidronic acid on the bond strength of calcium silicate-based cements after 1 and 21 days: an in vitro study. BMC Oral Health 2021; 21(1):591. doi: 10.1186/s12903-021-01959-5 [Crossref] [ Google Scholar]
- Ulusoy Ö, Ballal NV, Narkedamalli R, Ulusoy N, Shetty KP, Luke AM. Dislodgement resistance and structural changes of tricalcium silicate-based cements after exposure to different chelating agents. PLoS One 2024; 19(1):e0296647. doi: 10.1371/journal.pone.0296647 [Crossref] [ Google Scholar]
- Alamoudi RA, Abu Zeid ST. Effect of irrigants on the push-out bond strength of two bioceramic root repair materials. Materials (Basel) 2019; 12(12):1921. doi: 10.3390/ma12121921 [Crossref] [ Google Scholar]
- Ipek I, Karaağaç Eskibağlar B, Yildiz Ş, Ataş O, Ünal M. Analysis of the bond strength between conventional, putty or resin-modified calcium silicate cement and bulk fill composites. Aust Dent J 2023; 68(4):265-72. doi: 10.1111/adj.12977 [Crossref] [ Google Scholar]
- da Silva EJ, Carvalho NK, Zanon M, Senna PM, De-Deus G, Zuolo ML. Push-out bond strength of MTA HP, a new high-plasticity calcium silicate-based cement. Braz Oral Res 2016; 30(1):e84. doi: 10.1590/1807-3107BOR-2016.vol30.0084 [Crossref] [ Google Scholar]