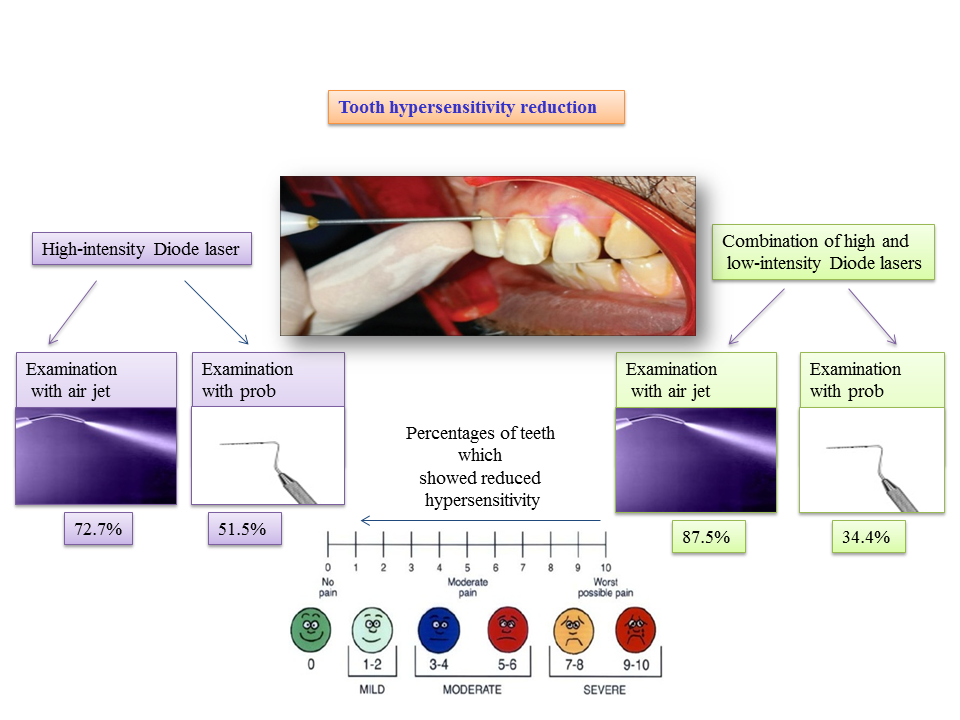
Visual Abstract
JODDD now with visual abstracts. Authors can now add a visual abstract to their submission.
Platinum* Open Access
*This Platinum Open Access journal publishes articles totally free of charge for the authors and provides unrestricted access to the published content through its website and open access repositories such as PubMed Central.
Indexing & Abstracting





Following

Social media
